Reduce Inflammation with Yoga
By John M. de Castro, Ph.D.
“Yoga is an incredible resource to combat stress and promote healthy habits in body and mind. Many people cite stress reduction as their reason to practice yoga, and research has their back – reducing stress helps reduce inflammation.” – Amy Tenney
The immune system is designed to protect the body from threats like stress, infection, injury, and toxic chemicals. One of its tools is the Inflammatory response. This response works quite well for short-term infections and injuries. But when inflammation is protracted and becomes chronic, it can itself become a threat to health. It can produce autoimmune diseases such as colitis, Chron’s disease, arthritis, heart disease, increased cancer risk, lung disease, sleep disruption, gum disease, decreased bone health, psoriasis, and depression.
Needless to say, chronic inflammation can create major health problems. Indeed, the presence of chronic inflammation is associated with reduced longevity. So, it is important for health to control the inflammatory response, allowing it to do its job in fighting off infection but reducing its activity when no external threat is apparent. Of course, it is far better to prevent chronic inflammation in the first place than to treat it later. Mind-body techniques such as yoga have been shown to reduce the inflammatory response. The research is accumulating, so it is reasonable to summarize what has been discovered.
In today’s Research News article “Impact of Yoga on Inflammatory Biomarkers: A Systematic Review.” (See summary below or view the full text of the study at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6700894/), Djalilova and colleagues review and summarize the published research literature on the effects of yoga practice on biomarkers of inflammation in adults. They found 15 published studies with 10 randomized controlled trials, including a total of 957 participants. Yoga practice was majority Hatha yoga and occurred from 8 weeks to 6 months.
They found that 11 of the 15 studies reported significant decreases in inflammatory biomarkers IL-6, CRP, and TNF-α. These reductions occurred in patients with cancer, cardiovascular disease, chronic stress, arthritis, and hypertension. The studies that did not see improvements included less than 1000 minutes of practice. All but 1 study with practice between 1000 to 4500 minutes found significant improvements in inflammation.
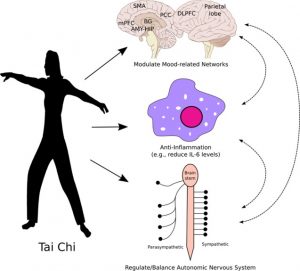
Hence, the published research found yoga to be a safe and effective treatment to reduce the inflammatory response in patients with a wide variety of medical conditions. It appears that at least a total of 1000 minutes of practice is required for effectiveness. It is not known what the mechanisms might be by which yoga practice reduces inflammation. But, it can be speculated that it may do so by reducing stress effects, as stress is known to promote inflammation, or it may work by improving autonomic nervous system activity that is also known to promote inflammation.
Regardless of the mechanism, the published research to date supports the use of yoga practice to reduce inflammation in patients with a wide variety of diseases. Since, inflammation generally exacerbates the symptoms of their diseases, yoga practice may then improve their symptoms, reduce their suffering, increase longevity, and improve their quality of life.
So, reduce inflammation with yoga.
“A number of studies have suggested that yoga and meditation – along with other mind/body activities – can reduce inflammation as well as influence some immunological markers of stress.” – Andrew Weil
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Google+ https://plus.google.com/106784388191201299496/posts and on Twitter @MindfulResearch
Study Summary
Djalilova, D. M., Schulz, P. S., Berger, A. M., Case, A. J., Kupzyk, K. A., & Ross, A. C. (2019). Impact of Yoga on Inflammatory Biomarkers: A Systematic Review. Biological research for nursing, 21(2), 198–209. https://doi.org/10.1177/1099800418820162
Abstract
Background:
Many chronic conditions, including heart disease, cancer, and rheumatoid arthritis, are associated with underlying chronic inflammatory processes. Literature reviews have analyzed a variety of integrative therapies and their relationships with chronic inflammation. This systematic review is unique in reporting solely on yoga’s relationship with inflammation. Its purpose was to synthesize current literature examining the impact of yoga interventions on inflammatory biomarkers in adults with chronic inflammatory–related disorders.
Method:
Searches of several electronic databases were conducted. Inclusion criteria were (a) English language, (b) sample age >18 years old, (c) yoga interventions involving postures with or without yoga breathing and/or meditation, and (d) measured inflammatory biomarkers.
Results:
The final review included 15 primary studies. Of these, seven were rated as excellent and eight as average or fair. There was considerable variability in yoga types, components, frequency, session length, intervention duration, and intensity. The most common biomarkers measured were interleukin-6 (n = 11), C-reactive protein (n = 10), and tumor necrosis factor (n = 8). Most studies reported positive effects on inflammatory biomarkers (n = 11) from baseline to post yoga intervention. Analysis of the dose showed higher total dose (>1,000 min) resulted in greater improvements in inflammation.
Conclusion:
This review suggests that yoga can be a viable intervention to reduce inflammation across a multitude of chronic conditions. Future studies with detailed descriptions of yoga interventions, measurement of new and well-established inflammatory biomarkers, and larger sample sizes are warranted to advance the science and corroborate results.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6700894/