By John M. de Castro, Ph.D.
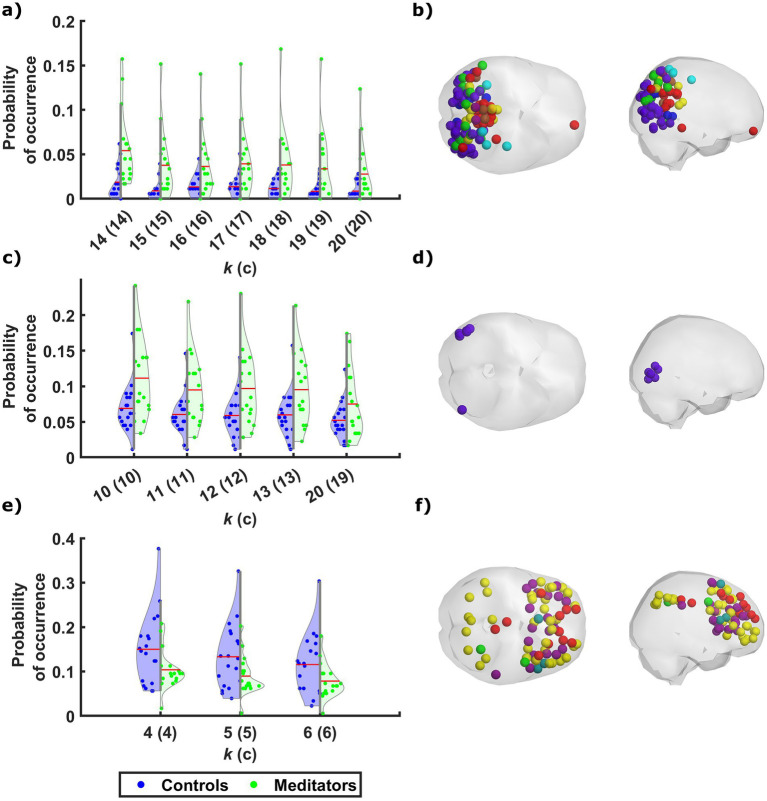
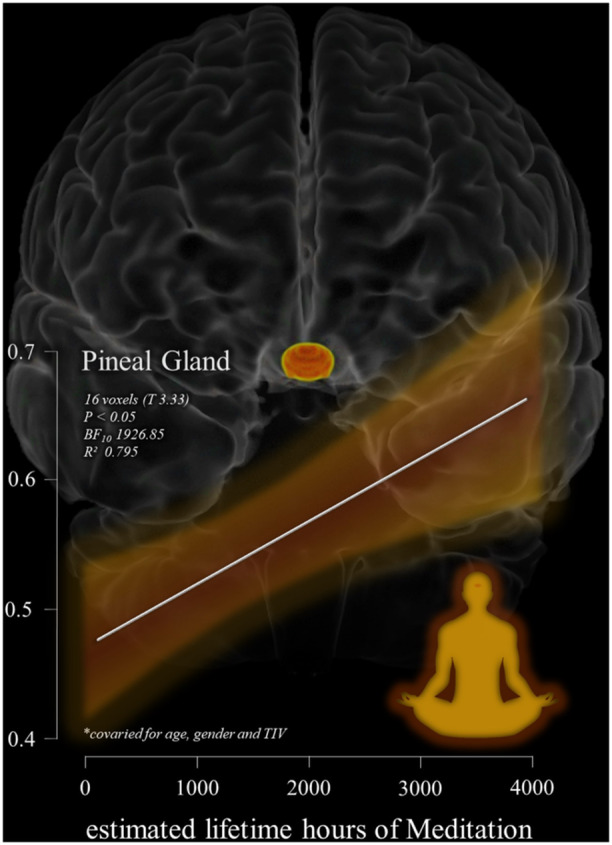
In today’s Research News article “Long-term mindfulness meditation increases occurrence of sensory and attention brain states” (See summary below or view the full text of the study at: https://pmc.ncbi.nlm.nih.gov/articles/PMC11743700/ ) Panitz and colleagues examined brain activity in experienced meditators in comparison to meditation naive participants. They report that at rest the brains of experienced meditators had enhanced activity in the visual and dorsal attention networks. This suggests that long-term meditation practice shifts the brain to emphasize immediate stimulus environments.
Meditation changes the brain toward processing of the more immediate sensory environment.
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on the Contemplative Studies Blog http://contemplative-studies.org
Study Summary
Panitz DY, Mendelsohn A, Cabral J, Berkovich-Ohana A. Long-term mindfulness meditation increases occurrence of sensory and attention brain states. Front Hum Neurosci. 2025 Jan 6;18:1482353. doi: 10.3389/fnhum.2024.1482353. PMID: 39834400; PMCID: PMC11743700.
Abstract
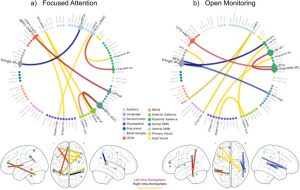
Interest has been growing in the use of mindfulness meditation (MM) as a therapeutic practice, as accumulating evidence highlights its potential to effectively address a range of mental conditions. While many fMRI studies focused on neural activation and functional connectivity during meditation, the impact of long-term MM practice on spontaneous brain activity, and on the expression of resting state networks over time, remains unclear. Here, intrinsic functional network dynamics were compared between experienced meditators and meditation-naïve participants during rest. Our analysis revealed that meditators tend to spend more time in two brain states that involve synchrony among cortical regions associated with sensory perception. Conversely, a brain state involving frontal areas associated with higher cognitive functions was detected less frequently in experienced meditators. These findings suggest that, by shifting attention toward enhanced sensory and embodied processing, MM effectively modulates the expression of functional network states at rest. These results support the suggested lasting effect of long-term MM on the modulation of resting-state networks, reinforcing its therapeutic potential for disorders characterized by imbalanced network dynamics. Moreover, this study reinforces the utility of analytic approaches from dynamical systems theory to extend current knowledge regarding brain activity and evaluate its response to interventions.



 Mindfulness Meditation Reduces Pain.
Mindfulness Meditation Reduces Pain.