Improve Education Students Psychological Well-Being with Mindfulness
By John M. de Castro, Ph.D.
“Mindfulness practices help anchor the mind, creating space to become aware of our thoughts and feelings, and keeps us in the present moment, all of which helps reduce stress and anxiety and boosts levels of attention and concentration.” – Rebecca Enderby
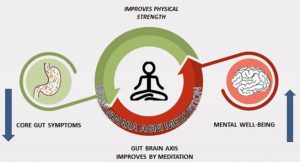
In the modern world education is a key for success. There is a lot of pressure on university students to excel so that they can get the best jobs after graduation. The pressure can lead to stress, anxiety, and depression which can impede the student’s mental health, well-being, and school performance. But it is, for the most part, beyond the ability of the individual to change the environment to reduce stress, so it is important that methods be found to reduce the college students’ responses to stress; to make them more resilient when high levels of stress occur. Contemplative practices including meditation, mindfulness training, exercise, Tai Chi and Qigong, and yoga practice have been shown to reduce the psychological and physiological responses to stress, relieve anxiety, and reduce depression
In today’s Research News article “The Effects of a Mindfulness Program on Mental Health in Students at an Undergraduate Program for Teacher Education: A Randomized Controlled Trial in Real-Life.” (See summary below or view the full text of the study at: https://www.frontiersin.org/articles/10.3389/fpsyg.2021.722771/full?utm_source=F-AAE&utm_medium=EMLF&utm_campaign=MRK_1790561_a0P58000000G0YfEAK_Psycho_20211214_arts_A ) Juul and colleagues recruited teacher education college students and randomly assigned them to a wait-list control condition or to receive 8 weekly 2.5 hour sessions of the Mindfulness-Based Stress Reduction (MBSR) program. The program consists of training in meditation, body scan, and yoga, group discussion, and daily home practice. They were measured before and after training and 3 months later for perceived stress, anxiety, depression, well-being, resilience, mindfulness, and resting state cognitive activity.
They found that in comparison to baseline and the wait-list control group, the group that received Mindfulness-Based Stress Reduction (MBSR) had significantly higher well-being and significantly lower levels of perceived stress, anxiety, depression, and resting state cognitive activity of distracting thoughts, thoughts of self and comfort. In addition, they found that the effect of MBSR on perceived stress was in part mediated by resting state cognitive activity of distracting thoughts and comfort and by thoughts of self on anxiety and depression. These effects were still present at the 3-month follow-up measurement.
The study demonstrates that mindfulness training improves the mental health of stresses teacher education college students. It has been routinely shown in previous research with a variety of groups that mindfulness training produces reduced levels of perceived stress, anxiety, and depression and increased levels of well-being. The new finding is that these improvements in mental health produced by the mindfulness training appear to be in part mediated by changes in the students’ resting state cognitive activity. In other words, the training appears to alter the mental contents of the students which in turn improves their mental health. The mindfulness trained students appear to have fewer distracting thoughts, thoughts of self and comfort and these reductions appear to improve their psychological well-being.
So, improve education students psychological well-being with mindfulness.
“It’s no secret that college can quickly become a major stressor for many students. Balancing multiple classes on top of work, a social life, and a million other things is a lot to take on at once. Don’t let yourself become too overwhelmed with everything. Instead, try . . . mindfulness.” – Savannah Byers
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are available on Twitter @MindfulResearch
Study Summary
Juul L, Brorsen E, Gøtzsche K, Nielsen BL and Fjorback LO (2021) The Effects of a Mindfulness Program on Mental Health in Students at an Undergraduate Program for Teacher Education: A Randomized Controlled Trial in Real-Life. Front. Psychol. 12:722771. doi: 10.3389/fpsyg.2021.722771
Background: In this study, we aimed to investigate the effects of a mindfulness program including Mindfulness-Based Stress Reduction (MBSR) on the mental health of student teachers when offered at their educational institution in a real-life context.
Methods: A parallel randomized controlled trial (RCT) was conducted among self-selected student teachers at a Danish undergraduate program for teacher education in the autumns of 2019 and 2020. Participation was not recommended in case of (1) clinical depression or a diagnosis of psychosis or schizophrenia, (2) abuse of alcohol, drugs, and/or medicine. Randomization was performed by a Statistician who was blinded to the identity of the students. Data was collected using self-reported questionnaires. The primary outcome was a change in perceived stress 3 months from baseline. Secondary outcome measures were symptoms of anxiety and depression, well-being, resilience, mindfulness, and thoughts and feelings during rest. The effects were analyzed according to the intention-to-treat principle using mixed-effect linear regression models. Mediating effects of mindfulness skills on the mental health outcomes were explored using structural equation modeling.
Results: The study group included 67 student teachers with 34 allocated to the intervention group (median age: 25 years; women: n = 24, 71%); and 33 students (median age: 25 years; women: n = 25, 76%) allocated to a waiting list control group. At baseline, mean Perceived Stress Scale (PSS) scores were 18.88 (SD: 5.75) in the intervention group and 17.91 (SD: 6.36) in the waiting list control group. A total of 56 students completed the questionnaire at a 3-month follow-up (28 in both the intervention- and the control group). Statistically significant effects of the intervention were found on perceived stress, symptoms of anxiety and depression, well-being, and on three of seven resting-state dimensions. No effects were found on resilience or mindfulness. Statistically significant mediated effects via resting-state dimensions were found.
Conclusion The findings suggested that offering a mindfulness program at an undergraduate program for teacher education could significantly improve the mental health among self-selected students within 3 months. Results of mediation analysis supported the hypothesis that some of the effects might be explained by reduced distracting thoughts.