Improve Gastrointestinal Health with Meditation
By John M. de Castro, Ph.D.
“Humans were never designed to be stressed out all the time, and when we learn to calm our nervous systems, our health improves dramatically. Our nervous system and the gut are inextricably linked.” – Buffy Owens
Stress affects gastrointestinal function. Short-term stress can produce a loss of appetite and slow digestion while long-term stress can produce heartburn, indigestion, nausea and vomiting, diarrhea, constipation and associated lower abdominal pain. Mindfulness is known to be helpful in reducing the psychological and physical responses to stress and contemplative practice has been shown to improve the symptoms of Irritable Bowel Syndrome and dyspepsia. In addition, mindfulness practices improve the intestinal bacteria that are important for digestion. So, it is likely that meditation practice would improve gastrointestinal health.
In today’s Research News article “Improvement in Gastrointestinal Quality of Life Index (GIQLI) following meditation: An open-trial pilot study in India.” (See summary below or view the full text of the study at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8039347/ ) Kanchibhotla and colleagues recruited healthy adults and had them engage in daily 20-minute meditation for 50 days. The practice was a focused meditation on the gut region. They were measured before, at 24 days and after the intervention period for gastrointestinal quality of life divided into five domains: core symptoms, physical, psychological, social, and disease specific.
They found that after 24 and 50 days of meditation practice there were significant improvements with large effect sizes in gastrointestinal quality of life, including all domains. There were some indications that the effects were larger for men than women. Clearly, there were large significant improvements after meditation in gastrointestinal function.
It should be kept in mind that this was a pilot study that lacked a comparison (control) condition leaving open a wide variety of confounding alternative interpretations such as expectancy effects, attention (Hawthorne) effects, experimenter bias, etc. But better controlled studies have reported that mindfulness improves gastrointestinal function. So, it is likely that in the present study the meditation practice improved gastrointestinal function. But future better controlled research is needed.
So, improve gastrointestinal health with meditation.
“In calming your stress response, meditation can help prevent the slowed digestion speed, altered gene expression, intestinal permeability, and disruptive changes to gut microbes caused by stress.” – Crystal Starr
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are available on Twitter @MindfulResearch
Study Summary
Kanchibhotla, D., Sharma, P., & Subramanian, S. (2021). Improvement in Gastrointestinal Quality of Life Index (GIQLI) following meditation: An open-trial pilot study in India. Journal of Ayurveda and integrative medicine, 12(1), 107–111. https://doi.org/10.1016/j.jaim.2021.01.006
Abstract
Background
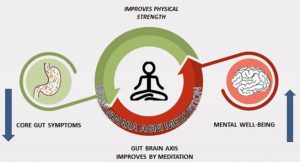
Medical science is increasingly recognizing the role of gut health in achieving optimal wellbeing. A healthy gut improves digestion. Additionally, it has a positive impact on multiple physiological networks such as immune system, central nervous system and hepato-endocrine system, thus contributing to the overall quality of life. Functional gastrointestinal disorders: also known as disorders of gut-brain interaction, such as irritable bowel syndrome are increasing worldwide. Conditions like stress, anxiety and mental disorders are correlated with these disorders. Mind-body interventions have been shown to ameliorate stress, anxiety and related conditions that may aggravate functional gastrointestinal disorders.
Objective
The present study aims to investigate the benefits of a novel meditation technique called the Vaishvanara Agni meditation (VAM) on the gastrointestinal quality of life.
Materials and methods
54 subjects participated in the study and practiced VAM for 50 days. During the Vaishvanara Agni meditation (VAM), attention is directed to the navel region and the digestive system. The effect of the meditation was evaluated using the gastrointestinal quality of life (GI-QoL) questionnaire, which was administered to subjects at three different time points i.e. day 0, day 24 and day 50.
Results
GI-QoL was significantly improved with the practice of VAM. Additionally, significant improvements were noticed in all sub domains especially core symptoms, physical strength and the psychological domain.
Conclusion
Meditation practices that focus on improving digestion can be an effective tool for improving gut health.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8039347/