By John M. de Castro, Ph.D.
In today’s Research News article “Consumer-Grade Neurofeedback With Mindfulness Meditation: Meta-Analysis” (See summary below or view the full text of the study at: https://pmc.ncbi.nlm.nih.gov/articles/PMC12046271/) Treves and colleagues reviewed, summarized, and performed a meta-analysis of the published research studies on the effectiveness of neurofeedback, produced by a readily available commercial neurofeedback device, on mindfulness, and physiological and psychological health. They report that the published findings found only a small positive effect on psychological distress but, in general, no effects on mindfulness or physiological and psychological health.
Neurofeedback does no improve mindfulness.
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on the Contemplative Studies Blog http://contemplative-studies.org
Study Summary
Treves I, Bajwa Z, Greene KD, et al. Consumer-Grade Neurofeedback With Mindfulness Meditation: Meta-Analysis. J Med Internet Res. 2025;27:e68204. Published 2025 Apr 17. doi:10.2196/68204
Abstract
Background
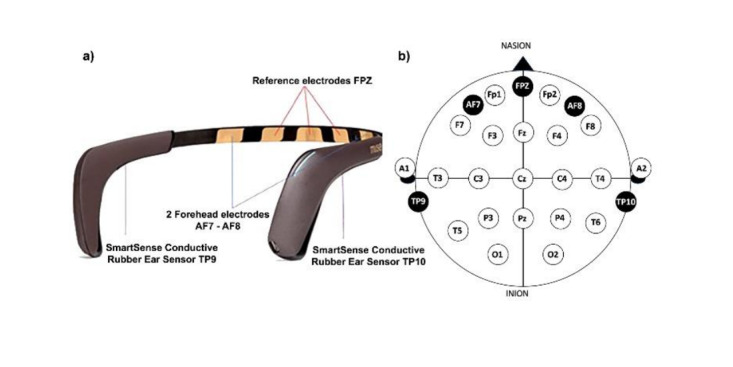
There is burgeoning interest in the application of neuroscientific technology to facilitate meditation and lead to beneficial psychological outcomes. One popular approach is using consumer-grade neurofeedback devices to deliver feedback on brain targets during meditation (mindfulness-based neurofeedback). It is hypothesized that optimizing brain targets like alpha and theta band activity may allow meditators to experience deeper mindfulness and thus beneficial outcomes.
Objective
This study aimed to systematically review and meta-analyze the impacts of consumer-grade mindfulness-based neurofeedback compared with control conditions. Included studies involved mindfulness practice operationalized as open monitoring or focused attention meditation. This study was preregistered.
Methods
A total of 16 randomized controlled training trials, as well as 5 randomized within-participant designs were included, encompassing 763 and 167 unique participants, respectively. Effects were categorized outcomes (ie, psychological distress, cognitive function, and physiological health) and process variables (ie, state mindfulness and brain measures). Study risk of bias, reporting bias, and publication bias were assessed.
Results
Samples were typically small (n=30-50), and the majority of studies used mindfulness apps as controls. To deliver neurofeedback, most studies used the Muse device (11/16 randomized controlled trials [RCTs]). There was a modest effect for decreases in psychological distress compared with controls (k=11, g=–0.16, P=.03), and heterogeneity was low (I2< 0.25). However, there was no evidence for improvements in cognition (k=7, g=0.07, P=.48), mindfulness (k=9, g=0.02, P=.83), and physiological health (k=7, g=0.11, P=.57) compared to controls. Mechanistic modulation of brain targets was not found in RCTs or within-participant designs. Sex (male or female), age, clinical status, study quality, active or passive controls, sample size, and neurofeedback duration did not moderate effects. There was some evidence for reporting bias, but no evidence of publication bias. Adverse effects were not assessed in 19 out of 21 studies and not found in the 2 studies that assessed them.
Conclusions
Assertions that consumer-grade devices can allow participants to modulate their brains and deepen their meditations are not currently supported. It is possible that neurofeedback effects may rely on “neurosuggestion” (placebo effects of neurotechnology). Future research should examine more extensive calibration and individualization of devices, larger sample sizes, and gold-standard sham-controlled RCTs.