There is an accumulating volume of research findings to demonstrate that Mind-body therapies have highly beneficial effects on the health and well-being of humans. These include meditation, yoga, tai chi, qigong, biofeedback, progressive muscle relaxation, guided imagery, hypnosis, and deep breathing exercises. Because of their proven benefits the application of these practices to relieving human suffering has skyrocketed.
It is clear that Mind-body therapies affect the physiology. In other words, the mind can alter the body. In turn, the genes can affect our minds. In fact, the genes have been shown to affect an individual’s inherent level of mindfulness (see http://contemplative-studies.org/wp/index.php/category/research-news/genetics/). These interactions are well documented. The mechanisms by which they occur, however, are not well understood. It has been shown that contemplative practices help create balance in the inflammatory response (see http://contemplative-studies.org/wp/index.php/category/research-news/inflammatory-response/) which is very beneficial for health. But, the mechanism through which contemplative practices affect the immune system is not known.
The genes dictate all of the chemical processes in our bodies including immune and inflammatory responses. So, it would seem reasonable to investigate whether alterations in gene expressions might be the intermediary between mind-body therapies and health. In today’s Research News article “Functional Genomics in the Study of Mind-Body Therapies”
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4295747/
Niles and colleagues review the literature on the effects of mind-body therapies on the functional expression of the genes. Out of the vast number of genomic pathways that can be affected, they found one which appears to be altered by mind-body therapies in general. This was a reduction in activity (downregulation) of the expression of genes that elicit the inflammatory response. In other words mindfulness practices reduce inflammation by reducing the activity of the genes that produce it.
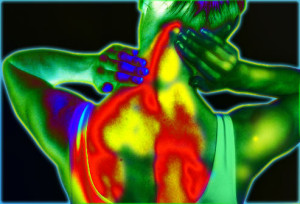
This finding is extremely important as an overactive inflammatory system underlies many chronic diseases. Inflammation is a normal response of the body to outside threats like stress, infection, injury, and toxic chemicals. It is designed to protect the body and ward off these threats. It works quite well for short-term infections and injuries and as such is an important defense mechanism for the body. But when inflammation is protracted and becomes chronic, it can itself become a threat to health. Chronic inflammation can produce autoimmune diseases such as colitis, Chron’s disease, arthritis, heart disease, increased cancer risk, lung disease, sleep disruption, gum disease, decreased bone health, psoriasis, and depression. Needless to say chronic inflammation can create major health problems. Indeed, the presence of chronic inflammation is associated with reduced longevity. So, it is important for health to control the inflammatory response, allowing it to do its job in fighting off infection but then reducing its activity when no external threat is apparent. Mind-body therapies appear to do just that by reducing the expression of the genes that produce inflammation.
Niles and colleagues also found that a number of mind-body therapies increase the activity of telomerase, an enzyme that protects the genes from deterioration, particularly during aging. Hence, mind-body therapies appear to have anti-aging properties by increasing the activity of genes the reduce age related deterioration (see http://contemplative-studies.org/wp/index.php/2015/07/17/aging-healthily-yoga-and-cellular-aging/).
All of these results suggest that mind-body therapies promote health and well-being by altering gene expression. This is interesting and important. The next question is what are the mechanisms by which these practices affect gene expressions? It will be up to future research to investigate this link in the causal chain from mind-body therapies to the promotion of health and well-being.
So engage in mind-body practices, change gene expression and promote health and well-being.
“Our genes are quite dynamic in their expression and …. the calmness of our mind can actually have a potential influence on their expression.” – Richard Davidson
CMCS – Center for Mindfulness and Contemplative Studies