By John M. de Castro, Ph.D.
In today’s Research News article “Yoga an integrated mind body intervention for improvement in quality of life in individuals with Alzheimer’s disease and their caregivers” (See summary below or view the full text of the study at: https://pmc.ncbi.nlm.nih.gov/articles/PMC11968721/) Kaushik and colleagues investigated the effects of a 12-week yoga practice intervention on depression, cognitive abilities and quality of life of patients with Alzheimer’s Disease and the difficulties of caregiving. They report that yoga practice significantly reduced depression and increased cognitive ability and quality of life in the patients and significantly reduced the burden of caregiving.
Yoga practice improves the symptoms of patients with Alzheimer’s disease and their caregivers difficulties.
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on the Contemplative Studies Blog http://contemplative-studies.org
Study Summary
Kaushik M, Yadav A, Upadhyay A, et al. Yoga an integrated mind body intervention for improvement in quality of life in individuals with Alzheimer’s disease and their caregivers. Front Aging. 2025;6:1449485. Published 2025 Mar 21. doi:10.3389/fragi.2025.1449485
Abstract
Background and objective
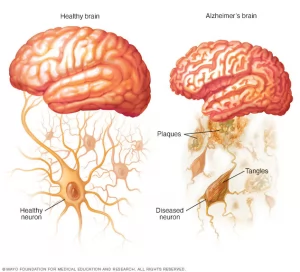
Alzheimer’s disease (AD) presents profound challenges, significantly impairing quality of life (QOL) for patients and increasing the burden on caregivers. This study aims to investigate the effectiveness of a tailored 12-week yoga intervention in improving the quality of life for individuals with mild to moderate AD and reducing caregiver burden (CB).
Methods
This is yoga interventional study with healthy controls enrolled 30 participants (18 males, 12 females) diagnosed with mild to moderate AD by an expert neurologist. Participants were aged 60 years or older and were recruited from an old age home. A 12-week yoga program, including specific postures (asanas), pranayama (breathing exercises), and meditation, was conducted for 1 hour daily, 6 days a week. Neurocognitive assessments were performed pre- and post-intervention using the Geriatric Depression Scale (GDS), Montreal Cognitive Assessment (MoCA), and Caregiver Burden (CB) Scale. MoCA scores were analyzed across specific domains, including language, memory, attention, visuospatial ability, delayed recall, abstraction, and orientation.
Results
The intervention led to significant improvements in quality-of-life measures. GDS scores decreased from 8.36 ± 2.79 to 5.13 ± 3.07 (P < 0.01; 95% CI: −3.98 to −2.31), while MoCA total scores improved from 18.23 ± 4.90 to 21.10 ± 5.09 (P < 0.01; 95% CI: 2.17–3.89). Domain-specific MoCA scores also showed significant enhancements, particularly in language, attention, and delayed recall. Caregiver burden, measured using the CB Scale, demonstrated notable reductions following the intervention (P < 0.01; 95% CI: −2.54 to −1.23).
Conclusion
This study underscores the significant improvements in depression and cognitive function, and overall quality of life in individuals with mild to moderate AD. Additionally, the intervention alleviated caregiver burden, highlighting its potential as an effective mind-body approach for AD management.