Improve College Student Psychological Well-Being with Mindfulness and Relaxation
By John M. de Castro, Ph.D.
“mindfulness helps focus by tuning out distractions, improving memory, decision-making and attention skills. . . It is not a panacea; it is not for everyone. However, it is very worth trying. It may be the next evolution in health care and well-being.” – Affordable Colleges
In the modern world education is a key for success. There is a lot of pressure on college students to excel so that they can get the best jobs after graduation. The pressure can lead to stress, anxiety, and depression which can impede the student’s mental health, well-being, and school performance. So it is important that methods be found to reduce the college students’ responses to stress; to make them more resilient.
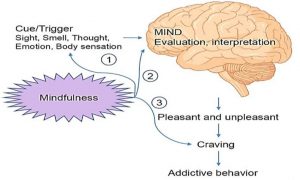
Contemplative practices including meditation, mindfulness training, exercise, Tai Chi and Qigong, and yoga practice have been shown to reduce the psychological and physiological responses to stress, relieve anxiety, and reduce depression . A therapeutic technique that contains mindfulness training and Cognitive Behavioral Therapy (CBT) is Acceptance and Commitment Therapy (ACT). It focuses on the individual’s thoughts, feelings, and behavior and how they interact to impact their psychological and physical well-being. It then works to change thinking to alter the interaction and produce greater life satisfaction. ACT employs mindfulness practices to increase awareness and develop an attitude of acceptance and compassion in the presence of painful thoughts and feelings. ACT teaches individuals to “just notice”, accept and embrace private experiences and focus on behavioral responses that produce more desirable outcomes. This suggests that ACT may be effective in improving the psychological well-being of college students.
In today’s Research News article “Effect of Acceptance and Commitment Therapy Combined with Music Relaxation Therapy on the Self-Identity of College Students.” (See summary below or view the full text of the study at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8853795/ ) Yin recruited college students and assigned them to receive either a 2-month program of Acceptance and Commitment Therapy (ACT) plus systematic muscle relaxation with music, or conventional self-identity intervention, including health education, regular communication, and regular follow-up. They were measured before and after the treatments for anxiety, depression, resilience, and quality of life.
They found that in comparison to baseline and the control condition Acceptance and Commitment Therapy (ACT) plus relaxation produced significant reductions in anxiety and depression and significant increases in resilience and quality of life. It cannot be determined if the combination of ACT and relaxation was necessary for the benefits or is each individually may have been effective.
So, improve college student psychological well-being with mindfulness and relaxation.
“mindfulness . . . can also be a great tool for students, reducing stress and increasing well-being and productivity.” – Rebecca Enderby
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Twitter @MindfulResearch
Study Summary
Yin J. (2022). Effect of Acceptance and Commitment Therapy Combined with Music Relaxation Therapy on the Self-Identity of College Students. Journal of healthcare engineering, 2022, 8422903. https://doi.org/10.1155/2022/8422903
Abstract
This paper analyzes various effects of acceptance and commitment therapy combined with music relaxation therapy on the self-identity of the college students. Through open recruitment and following the principle of voluntary and confidential, 80 college students were selected from our school, and then they were divided into two groups: the control group (40 cases) and the observation group (40 cases). The observation group received acceptance and commitment therapy combined with music relaxation therapy. For the control group, conventional mental health interventions were administered. Two months after intervention, psychological status, mental resilience, and quality of life scores were compared between the two groups. Before intervention, there was no significant difference in SAS and SDS scores between the two groups (P > 0.05). After intervention, SAS and SDS scores were significantly higher than those in the control group, and the difference between the two groups was statistically significant (P < 0.05). Before intervention, there was no significant difference in the scores of toughness, strength, and optimism between the two groups (P > 0.05). After intervention, the scores of toughness, strength, and optimism in the two groups were all improved, and the scores of mental resilience in the observation group were higher than those in the control group, with statistical significance (P < 0.05). Before intervention, there was no significant difference in the quality of life scores between the observation group and the control group (P > 0.05). After intervention, the quality of life score of the observation group was higher than that of the control group, and the difference between the two groups was statistically significant (P < 0.05). The combined application of acceptance and commitment therapy and music relaxation therapy can help college students to improve their mental state, improve their mental resilience, enhance their evaluation of life quality, improve their sense of self-identity, and reduce the probability of the occurrence of unhealthy emotions such as depression.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8853795/