Improve Psychological Health During Addiction Recovery with Qigong
By John M. de Castro, Ph.D.
“For people in the early stages of recovery whose emotions may be all over the map, Tai Chi can help stabilize moods, provide mental focus and clarity, and smooth out the rough spots. “ – Pinnacle
Substance abuse is a major health and social problem. There are estimated 22.2 million people in the U.S. with substance dependence. It is estimated that worldwide there are nearly ¼ million deaths yearly as a result of illicit drug use which includes unintentional overdoses, suicides, HIV and AIDS, and trauma. Obviously, there is a need to find effective methods to prevent and treat substance abuse. There are a number of programs that are successful at stopping the drug abuse, including the classic 12-step program emblematic of Alcoholics Anonymous. Unfortunately, the majority of drug and/or alcohol abusers relapse and return to substance abuse. Hence, it is important to find an effective method to both treat substance abuse disorders and to prevent relapses.
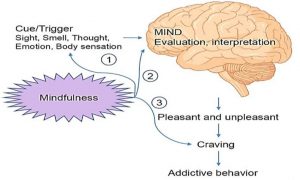
Mindfulness practices have been shown to improve recovery from various addictions. Tai Chi is a mindfulness practice that has documented benefits for the individual’s psychological and physical health and well-being. Tai Chi and Qigong are ancient mindfulness practices involving slow prescribed movements. Since Tai Chi and Qigong are both mindfulness practices and gentle exercises, that may be an acceptable and effective treatment for patients recovering from addictions. Studies on the use of Tai Chi and Qigong practices to treat substance abuse have been accumulating and there is a need to pause and summarize what has been learned.
In today’s Research News article “The Impact of Qigong and Tai Chi Exercise on Drug Addiction: A Systematic Review and Meta-Analysis.” (See summary below or view the full text of the study at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8957847/ ) Cui and colleagues review, summarize, and perform a meta-analysis of the published research studies on the effects of Tai Chi and Qigong practice during substance abuse treatment. They identified 11 studies including a total of 1072 participants.
They report that the published research found that Tai Chi and Qigong practices during substance abuse treatment produced significant reduction in depression, and anxiety, and significant improvements in quality of life, and sleep quality. Qigong practice appears to be superior to Tai Chi practice in producing these benefits.
Hence, the published research suggests that Tai Chi and Qigong practices improve the psychological health of the patients during addiction recovery.
“Tai chi can also be continued in life following treatment. It can serve as an important part of an aftercare plan that enhances well-being and reduces the likelihood of relapse.” – Footprints to Recovery
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Twitter @MindfulResearch
Study Summary
Cui, J., Liu, F., Liu, X., Li, R., Chen, X., & Zeng, H. (2022). The Impact of Qigong and Tai Chi Exercise on Drug Addiction: A Systematic Review and Meta-Analysis. Frontiers in psychiatry, 13, 826187. https://doi.org/10.3389/fpsyt.2022.826187
Abstract
Background
Previous preliminary studies have found that qigong exercises produced significant effects in healthy people and in various clinical populations. The purpose of this study was to systematically review the effects of qigong and tai chi exercise on individuals with drug addiction.
Methods
A systematic search of seven English databases and three Chinese databases was conducted to identify randomized controlled trials (RCTs) and non-randomized comparative studies (NRS) assessing the effects of qigong and tai chi on drug addiction. Study quality was assessed using the Checklist for the Evaluation of Non-Pharmaceutical Trial Reports (CLEAR-NPT).
Results
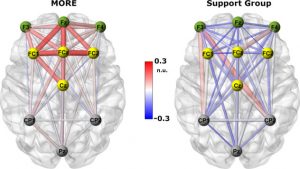
Two RCTs and nine NRS studies were included in this study, including a total of 1072 patients with drug addiction (age range, 27–43 years). The results showed that qigong and tai chi exercise had a significant overall effect on depression (SMD = −0.353, 95%CI [−0.548, −0.159]), anxiety (SMD = −0.541, 95%CI [−0.818, −0.264]), quality of life (SMD = 0.673, 95%CI [0.438, 0.907]), and sleep quality (SMD = −0.373, 95%CI [−0.631, −0.116]). The subgroup analysis found that qigong outperformed tai chi on the improving depression, anxiety, and sleep quality.
Conclusion
Existing studies suggest that qigong and tai chi are effective at improving depression, anxiety, and quality of life in drug users; however, the evidence from rigorous randomized controlled group trials is lacking.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8957847/