Improve generalized anxiety disorder with Mindfulness
By John M. de Castro, Ph.D.
“You can’t always control what goes on outside. But you can always control what goes on inside.” – Wayne Dyer
Anxiety disorders are the most common mental illness in the United States, affecting 40 million adults, or 18% of the population. The sufferer has recurring thoughts, such as impending disaster, that they may realize are unreasonable, but are unable to shake. Anxiety disorders have generally been treated with drugs. But there are considerable side effects, and these drugs are often abused. There are several psychological therapies for anxiety. But, about 45% of the patients treated do not respond to the therapy. So, there is a need to develop alternative treatments. Recently, it has been found that mindfulness training can be effective for anxiety disorders.
Mindfulness-Based Cognitive Therapy (MBCT) has been shown to be effective in treating anxiety disorders. MBCT involves mindfulness training, containing sitting, walking and body scan meditations, and cognitive therapy that attempts to teach patients to distinguish between thoughts, emotions, physical sensations, and behaviors, and to recognize irrational thinking styles and how they affect behavior. But it is unclear if MBCT will be effective for generalized anxiety disorder when delivered in a group setting.
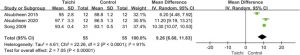
In today’s Research News article “Effects of group mindfulness-based cognitive therapy and group cognitive behavioural therapy on symptomatic generalized anxiety disorder: a randomized controlled noninferiority trial.” (See summary below or view the full text of the study at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9295460/ ) Jiang and colleagues recruited patients with generalized anxiety disorder and randomly assigned them to receive 8-weekly group sessions along with home practice of either Mindfulness-Based Cognitive Therapy (MBCT) or Cognitive Behavioral Therapy. They were measured before and after treatment and 3 months later for mindfulness, anxiety including psychiatric and somatic anxiety.
They found that both treatments successfully produce remission in a number of patients but Mindfulness-Based Cognitive Therapy (MBCT) produced significantly lower clinical symptom severity and significantly greater mindfulness and remissions at the end of therapy than Cognitive Behavioral therapy. But at the 3-month follow up there were no significant differences in remission rates.
Hence group-based mindfulness training improves generalized anxiety disorder to a greater extent than cognitive behavioral therapy alone immediately after treatment, but both were similarly effective 3 months later. This suggests that the efficient method of group therapy is effective in treating generalized anxiety disorder.
“Our anxiety does not come from thinking about the future, but from wanting to control it.” – Kahlil Gibran
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Twitter @MindfulResearch
Study Summary
Jiang SS, Liu XH, Han N, Zhang HJ, Xie WX, Xie ZJ, Lu XY, Zhou XZ, Zhao YQ, Duan AD, Zhao SQ, Zhang ZC, Huang XB. Effects of group mindfulness-based cognitive therapy and group cognitive behavioural therapy on symptomatic generalized anxiety disorder: a randomized controlled noninferiority trial. BMC Psychiatry. 2022 Jul 19;22(1):481. doi: 10.1186/s12888-022-04127-3. PMID: 35854250; PMCID: PMC9295460.
Abstract
Background
Mindfulness-based cognitive therapy (MBCT) is a promising alternative treatment for generalized anxiety disorder (GAD). The objective of this study was to examine whether the efficacy of group MBCT adapted for treating GAD (MBCT-A) was noninferior to group cognitive behavioural therapy (CBT) designed to treat GAD (CBT-A), which was considered one of first-line treatments for GAD patients. We also explored the efficacy of MBCT-A in symptomatic GAD patients compared with CBT-A for a variety of outcomes of anxiety symptoms, as well as depressive symptoms, overall illness severity, quality of life and mindfulness.
Methods
This was a randomized, controlled, noninferiority trial with two arms involving symptomatic GAD patients. Adult patients with GAD (n = 138) were randomized to MBCT-A or CBT-A in addition to treatment as usual (TAU). The primary outcome was the anxiety response rate assessed at 8 weeks after treatment as measured using the Hamilton Anxiety Scale (HAMA). Secondary outcomes included anxiety remission rates, scores on the HAMA, the state-trait anxiety inventory (STAI), the Hamilton Depression Scale (HAMD), the Severity Subscale of the Clinical Global Impression Scale (CGI-S), and the 12-item Short-Form Health Survey (SF-12), as well as mindfulness, which was measured by the Five Facet Mindfulness Questionnaire (FFMQ). Assessments were performed at baseline, 8 weeks after treatment, and 3 months after treatment. Both intention-to-treat (ITT) and per-protocol (PP) analyses were performed for primary analyses. The χ2 test and separate two-way mixed ANOVAs were used for the secondary analyses.
Results
ITT and PP analyses showed noninferiority of MBCT-A compared with CBT-A for response rate [ITT rate difference = 7.25% (95% CI: -8.16, 22.65); PP rate difference = 5.85% (95% CI: − 7.83, 19.53)]. The anxiety remission rate, overall illness severity and mindfulness were significantly different between the two groups at 8 weeks. There were no significant differences between the two groups at the 3-month follow-up. No severe adverse events were identified.
Conclusions
Our data indicate that MBCT-A was noninferior to CBT-A in reducing anxiety symptoms in GAD patients. Both interventions appeared to be effective for long-term benefits.