Personality Modulates the Effectiveness and Continued Use of Mindfulness Training
By John M. de Castro, Ph.D.
“Mindfulness-Based Stress Reduction is a formal eight-week program with a daylong intensive. This program is in over 250 hospitals around the country and many more around the world supporting people with stress, anxiety, depression, chronic pain, alleviating stress related to medical conditions and much more.” – Will Baum
Personality characteristics are thought to be relatively permanent traits that form an individual’s distinctive character. Current psychological research and theorization on personality has suggested that there are five basic personality characteristics. The so called “Big 5” are Extraversion, Agreeableness, Openness to Experience, Conscientiousness, and Neuroticism. Extraversion involves engagement with the external world, particularly other people. Agreeableness involves trust and helpfulness and a positive temperament. Openness to Experience is intellectual curiosity and is associated with creativity and a preference for novelty and variety. Conscientiousness involves planning, organization, dependability and self-discipline. Finally, Neuroticism involves moodiness, negative emotions, and a tendency to perceive even minor things as threatening or impossible. It is thought that most individual personalities can be captured by these five characteristics.
Measuring personality traits is only useful if it can predict the future behavior of the individual. Engaging in mindfulness training has been shown to have a large number of beneficial effects on the psychological, emotional, and physical health of the individual and is helpful in the treatment of mental and physical illness. It would be useful to be able to predict who would be most likely to participate fully and thereby benefit most from mindfulness training. It is possible that personality traits are good predictors of successful participation. So, it would be important to look to see if people high in some of these “Big 5” traits are more likely to engage in the program and continue practice even after the end of the formal program.
In today’s Research News article “Personality Predicts Utilization of Mindfulness-Based Stress Reduction During and Post-Intervention in a Community Sample of Older Adults “.” (See summary below or view the full text of the study at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4860670/ ), Barkan and colleagues recruited elderly adults over the age of 60 years. They received a standard 8-week Mindfulness-Based Stress Reduction (MBSR) program that met once a week for 2 hours and near the end of the program for a 7-hour intensive retreat. They were also encouraged to practice at home during training and to continue practice after the end of the formal training. MBSR contains meditation, body scan, and yoga training. The participants were measured prior to training for “Big 5” personality traits, perceived stress, and cognitive functioning. They maintained logs of their engagement in the MBSR sessions and activities throughout the program and 6 months after the end of the program.
Barkan and colleagues found that attendance at the MBSR training sessions was high at 94%. Further, they found that during the MBSR intervention, average weekly at home participation varied from 2.19 days/week for yoga to 3.56 days/week for body scanning. Importantly, they found that participants high in the “Big 5” personality trait of openness participated more frequently at home during the 8-week instruction period in meditation and body scanning and during the 6 months after in yoga, meditation and body scanning practices. Those participants who were high in agreeableness participated more frequently at home during the instruction period in meditation. None of the other three “Big 5” personality traits predicted participation rates.
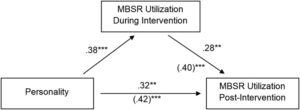
Employing a sophisticated regression analysis to the data, they found that the combination of openness and agreeableness predicted both participation during and following the end of formal training and participation during training predicted participation in the following 6 months. Hence, openness and agreeableness were associated with higher participation after training both directly and because they promoted participation during training that, in turn, was associated with increased later participation.
It is interested that the personality characteristics of the participant were associated with their rates of participation in MBSR both during and after training. This suggests that participants high in openness to experience would be most likely to participate in and benefit from the practice. The “Big 5” personality trait of openness to experience is associated with creativity and a preference for novelty and variety. Certainly, participation in MBSR would be novel for this elderly group. So, it is not surprising that openness to experience predicted participation.
“Do you have neurotic tendencies? You might give mindfulness a try. The practice has been shown to help quell the voice of the “obnoxious roommate” in your head. One of the “Big Five” personality traits, neuroticism is characterized by negative affect, rumination on the past and worry about the future, moodiness and loneliness. Practicing mindfulness may be a powerful way for people to detach from common characteristics of neuroticism, including obsessive negative thoughts and worries, and challenges regulating one’s emotions and behavior.” – Carolyn Gregoire
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Google+ https://plus.google.com/106784388191201299496/posts and on Twitter @MindfulResearch
Study Summary
Barkan, T., Hoerger, M., Gallegos, A. M., Turiano, N. A., Duberstein, P. R., & Moynihan, J. A. (2016). Personality Predicts Utilization of Mindfulness-Based Stress Reduction During and Post-Intervention in a Community Sample of Older Adults. Journal of Alternative and Complementary Medicine, 22(5), 390–395. http://doi.org/10.1089/acm.2015.0177
Abstract
Objectives: Mindfulness-based stress reduction (MBSR) is a promising intervention for older adults seeking to improve quality of life. More research is needed, however, to determine who is most willing to use the four techniques taught in the program (yoga, sitting meditation, informal meditation, and body scanning). This study evaluated the relationship between the Big Five personality dimensions (neuroticism, extraversion, openness to experience, conscientiousness, and agreeableness) and use of MBSR techniques both during the intervention and at a 6-month follow-up. The hypothesis was that those with higher levels of openness and agreeableness would be more likely to use the techniques.
Methods: Participants were a community sample of 100 older adults who received an 8-week manualized MBSR intervention. Personality was assessed at baseline by using the 60-item NEO Five-Factor Inventory. Use of MBSR techniques was assessed through weekly practice logs during the intervention and a 6-month follow-up survey. Regression analyses were used to examine the association between each personality dimension and each indicator of MBSR use both during and after the intervention.
Results: As hypothesized, openness and agreeableness predicted greater use of MBSR both during and after the intervention, while controlling for demographic differences in age, educational level, and sex. Openness was related to use of a variety of MBSR techniques during and after the intervention, while agreeableness was related to use of meditation techniques during the intervention. Mediation analysis suggested that personality explained postintervention MBSR use, both directly and by fostering initial uptake of MBSR during treatment.
Conclusions: Personality dimensions accounted for individual differences in the use of MBSR techniques during and 6 months after the intervention. Future studies should consider how mental health practitioners would use these findings to target and tailor MBSR interventions to appeal to broader segments of the population.