Reduce Compulsive Sexual Behavior with Mindfulness
By John M. de Castro, Ph.D.
“ve Sexual Behavior with Mindfulnessfeeling ashamed of one’s sexual desires, interests, fetishes, and so on, only makes one feel more obsessive and compulsive about them, rather than the opposite. . .. Mindfulness practice helps my clients to observe their reactions to themselves in accepting and non-judgmental ways. Also, they learn to catch and become aware of the negative thoughts and emotions that arise that make them feel compelled to act out.” – Michael Aaron
Sexual behavior is a very important aspect of human behavior, especially for reproduction. In fact, Sigmund Freud made it a centerpiece of his psychodynamic theory. At its best, it is the glue that holds families and relationships together. But, it is a common source of dysfunction and psychosocial problems. Compulsive sexual behavior “encompasses problems with preoccupation with thoughts surrounding sexual behavior, loss of control over sexual behavior, disturbances in relationships due to sexual behavior, and disturbances in affect (e.g., shame) due to sexual behavior.” It is also called sex addiction and hypersexuality. It is chronic and remarkably common affecting 3% to 17% of the population. In addition, it is associated with substance abuse in around half of people with compulsive sexual behavior.
Compulsive sexual behavior is frequently treated with psychotherapy, Cognitive Behavioral, Therapy, or drugs with mixed success. Since, it is also looked at as an addiction and mindfulness treatment has been found to be effective for both sexual dysfunction and for addictions, mindfulness may be affective for individuals with both substance abuse and compulsive sexual behavior. As a first step in evaluation this possibility, the relationship between mindfulness and compulsive sexual behavior needs to be investigated in these individuals.
In today’s Research News article “The relationship between mindfulness and compulsive sexual behavior in a sample of men in treatment for substance use disorders.” See summary below or view the full text of the study at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4996480/, Shorey and colleagues recruited men in a residential treatment center for substance abuse. Upon admission to the facility and after withdrawal from drugs the men completed a battery of tests including measures of mindfulness, alcohol use, drug use, and compulsive sexual behavior, including preoccupation, loss of control, relationship disturbance, and affect (emotional) disturbance.
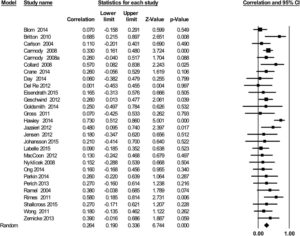
They found that the higher the level of mindfulness that the men had the lower the levels of drug use, alcohol use, and compulsive sexual behavior, including preoccupation, loss of control, relationship disturbance, and affect disturbance. These relationships with compulsive sexual behavior remained significant and negative even when drug and alcohol use were factored in. In contrast, drug use was not related to compulsive sexual behavior, except for a positive relationship with relationship disturbance. So, although there’s high comorbidity between substance abuse and compulsive sexual behavior, they don’t appear to be highly related.
These are encouraging results that suggest that mindfulness may be an antidote for compulsive sexual behavior in patients with substance abuse. These results, however, are correlative and so causation cannot be concluded and are only applicable to men. The next step, of course, will be to form a randomized clinical trial of the effects of mindfulness training on compulsive sexual behavior in patients with substance abuse in both men and women to establish the efficacy of mindfulness training as a treatment. It is possible that mindfulness training will be effective for the treatment of both substance abuse and compulsive sexual behavior in both genders.
So, reduce compulsive sexual behavior with mindfulness.
“findings tentatively support the usefulness of mindfulness in the effective treatment of sex addiction. In addition to helping bring about a reduction in dysfunctional sex-related actions, fantasies and thoughts, mindfulness training may help affected individuals gain improved emotional control, an increased ability to handle stressful situations and improved resistance to any potentially damaging sex-related urges that arise.” – The Ranch
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Google+ https://plus.google.com/106784388191201299496/posts and on Twitter @MindfulResearch
Study Summary
Shorey, R. C., Elmquist, J., Gawrysiak, M. J., Anderson, S., & Stuart, G. L. (2016). The relationship between mindfulness and compulsive sexual behavior in a sample of men in treatment for substance use disorders. Mindfulness, 7(4), 866–873. http://doi.org/10.1007/s12671-016-0525-9
Abstract
Substance use disorders (SUDs) are a serious worldwide problem. Despite years of research on the treatment of SUDs, relapse remains high. One factor that may complicate SUDs treatment for some patients is compulsive sexual behavior. Factors that are related to both SUDs and compulsive sexual behavior could be targeted in SUDs treatment. In the current study, we examined dispositional mindfulness, a protective factor for a range of mental health problems, and its relationship to compulsive sexual behavior in a SUDs treatment sample. This is the first study to examine this relationship in a SUDs sample. Medical records from men in residential SUDs treatment were reviewed for the current study (N = 271). Upon admission to treatment, men completed self-report measures on alcohol and drug use, dispositional mindfulness, and compulsive sexual behavior. Bivariate correlations demonstrated dispositional mindfulness to be negatively associated with a variety of indicators of compulsive sexual behavior. After controlling for alcohol and drug use and problems in hierarchical regression analyses, which were both associated with compulsive sexual behaviors, dispositional mindfulness remained negatively associated with all of the compulsive sexual behavior indicators. Our results provide the first empirical association between dispositional mindfulness and compulsive sexual behavior in a SUDs sample. Although continued research is needed in this area, our findings suggest that it may be beneficial for SUDs treatment to incorporate mindfulness-based interventions for individuals with comorbid compulsive sexual behavior.