Improve Walking in the Elderly with Knee Osteoarthritis with Tai Chi
By John M. de Castro, Ph.D.
“The most common type of arthritis is called osteoarthritis (OA). . . Fortunately, lifestyle changes such as gentle yoga have been shown to improve OA symptoms.” – Robin Madell
Osteoarthritis is a chronic degenerative joint disease that is the most common form of arthritis. It produces pain, swelling, and stiffness of the joints. It is the leading cause of disability in the U.S., with about 43% of arthritis sufferers limited in mobility and about a third having limitations that affect their ability to perform their work. Knee osteoarthritis effects 5% of adults over 25 years of age and 12% of those over 65. It is painful and disabling. Its causes are varied including, hereditary, injury including sports injuries, repetitive stress injuries, infection, or from being overweight.
There are no cures for knee osteoarthritis. Treatments are primarily symptomatic, including weight loss, exercise, braces, pain relievers and anti-inflammatory drugs, corticosteroids, arthroscopic knee surgery, or even knee replacement. Gentle movements of the joints with exercise and physical therapy appear to be helpful in the treatment of knee osteoarthritis. This suggests that alternative and complementary practices that involve gentle knee movements may be useful for treatment.
Mindfulness practices such as Tai Chi and Qigong and yoga have been shown to reduce the physical symptoms of knee osteoarthritis. Tai Chi practice, has been shown to be a safe and effective treatment for a wide variety of physical and psychological conditions, including arthritis. The research has been accumulating, so, it would seem reasonable to review and summarize what has been learned.
In today’s Research News article “Effects of Tai Chi exercise on improving walking function and posture control in elderly patients with knee osteoarthritis: A systematic review and meta-analysis.” (See summary below or view the full text of the study at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8078456/ ) You and colleagues review, summarize, and perform a meta-analysis of the effectiveness of Tai Chi practice on walking ability in elderly patients with knee osteoarthritis. They identified 11 published randomized controlled trials.
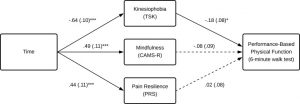
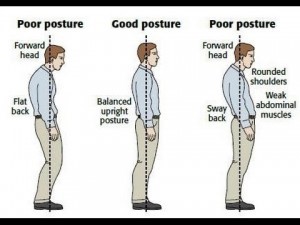
They report that the published research found that Tai Chi practice produced a significant improvement in the distance covered during a 6-minute walking test, faster performance with the timed up and go test, and improved postural control. Hence the published studies demonstrate that Tai Chi practice improves the walking ability of elderly patients with knee osteoarthritis. It should be mentioned, however, that they did not compare Tai Chi practice to other exercises. So, it cannot be determined as to whether Tai Chi practice produces its benefits as a result of exercise rather than something specific to Tai Chi practice.
Mobility is extremely important for the elderly. So, the improvement in walking ability should greatly contribute to their quality of life. In addition, improved walking ability should make falls less likely, and falls are a major contributor to disability and mortality in the elderly. So, Tai Chi practice should be recommended for elderly patients in general but particularly for patients with knee osteoarthritis.
So, improve walking in the elderly with knee osteoarthritis with Tai Chi.
“If you struggle with knee pain, yoga may offer relief. A regular exercise routine can help maintain good strength and mobility in the knees, which are crucial for walking and other daily activities” – Michelle Polizzi
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Google+ https://plus.google.com/106784388191201299496/posts and on Twitter @MindfulResearch
Study Summary
You, Y., Liu, J., Tang, M., Wang, D., & Ma, X. (2021). Effects of Tai Chi exercise on improving walking function and posture control in elderly patients with knee osteoarthritis: A systematic review and meta-analysis. Medicine, 100(16), e25655. https://doi.org/10.1097/MD.0000000000025655
Abstract
Objective:
It remains unclear whether Tai Chi is effective for walking function and posture control improvements in aged populations with knee osteoarthritis. The aim of this study was to systematically evaluate the effects of Tai Chi on improving walking function and posture control in elderly patients with knee osteoarthritis by updating the latest trial evidence.
Methods:
Web of Science, PubMed/Medline, Embase, Scopus, PEDro, and Cochrane library were searched up to October 1, 2020 to identify RCTs evaluating Tai Chi for improving walking function and posture control in older adults with knee osteoarthritis. The primary outcomes were walking function and posture control. Meta-analysis was performed with RevMan Version 5.3 software.
Results:
A total of 603 participants with knee osteoarthritis in the 11 trials were included. The results of meta-analysis showed that: The Tai Chi group was associated with better performance in 6-minute walk test (6 MWT), time up and go test (TUG) and “Western Ontario and McMaster Universities (WOMAC) Osteoarthritis Index” Physical Function Score than the control group ([MD: 46.67, 95% CI 36.91–56.43, P < .001]), ([MD: −0.89, 95% CI −1.16 to −0.61, P < .001]), ([MD: −11.28, 95% CI −13.33 to −9.24, P < .001]).
Conclusion:
This meta-analysis provided evidence from 11 RCTs that Tai Chi could be an excellent physical training strategy for improving walking function and posture control in older adults with knee osteoarthritis. Assuming that Tai Chi is at least effective and safe in most areas, it can be used as an adjuvant and reliable physical training strategy for walking function upgrading and balance control improvements for older patients with knee osteoarthritis.
What is known
Tai Chi exercise may potentially improve balance and reduce falls among the older adults. When it comes to elderly patients with specific knee osteoarthritis, its curative effects for walking function and postural control ability remain controversial.
What is new
The results of the meta-analysis with other new randomized controlled trials provide evidence support that Tai Chi Exercise has a positive effect on improving walking function and posture control in elderly patients with knee osteoarthritis. The present systematic review suggests that non-pharmaceutical therapies like Tai Chi could be used as an adjuvant and reliable physical training strategy for walking function upgrading and postural control improvements for older patients with knee osteoarthritis.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8078456/