Improve Physical Function in Chronic Pain Patients with Mind-Body Practice
By John M. de Castro, Ph.D.
“mind-body practices like tai chi, yoga, mindfulness and cognitive-behavioral therapy can all relieve lower back pain effectively.” – Wayne Jonas
We all have to deal with pain. It’s inevitable, but hopefully it’s mild and short lived. For a wide swath of humanity, however, pain is a constant in their lives. At least 100 million adult Americans have chronic pain conditions. The most common treatment for chronic pain is drugs. These include over-the-counter analgesics and opioids. But opioids are dangerous and highly addictive. Prescription opioid overdoses kill more than 14,000 people annually. So, there is a great need to find safe and effective ways to lower the psychological distress and improve the individual’s ability to cope with the pain.
There is an accumulating volume of research findings that demonstrate that mindfulness practices, in general, are effective in treating pain. Yoga practice has been shown to have a myriad of health benefits. These include relief of chronic pain. Yoga practice has also been shown to be effective for the relief of chronic pain. Other mind-body practices such as Tai Chi improves spinal health and reduces pain. Since mind body practices involve exercise, it would seem reasonable to look at the effectiveness of mind-body practices in improving physical function and relieving pain in chronic pain patients.
In today’s Research News article “Mind-Body Activity Program for Chronic Pain: Exploring Mechanisms of Improvement in Patient-Reported, Performance-Based and Ambulatory Physical Function.” (See summary below or view the full text of the study at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7872894/ ) Greenberg and colleagues recruited patients with chronic musculoskeletal pain and randomly assigned them to 10-week mind-body physical activity programs either with or without a Fitbit activity monitor. The programs consisted of 10 weekly 90-minute sessions teaching mindfulness, deep breathing, pain-specific cognitive behavioral skills, physical restoration skills, and education on the disability spiral. They were measured before and after training for physical function, disability, walking distance, and accelerometer-based steps, kinesiophobia (fear of movement due to pain), pain resilience, mindfulness, and pain catastrophizing.
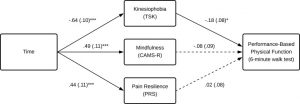
Using multilevel linear modelling, they found that compared to baseline, after treatment, there were significant increases in walking distance, step count, pain resilience and mindfulness, and a significant decrease in kinesiophobia and disability. Mediation analysis revealed that the improvement in disability was due to increases in pain resilience and mindfulness and decreases in kinesiophobia. For the walk test, only decreases in kinesiophobia mediated the improvement.
It should be noted that there wasn’t a control condition as both groups received the mind-body physical activity program. So, it is possible that confounds such as placebo effects and time-based healing may be operative. So, conclusions must be reached with caution. That being said, the results suggest that mind-body physical activity program improves physical function in chronic pain patients. The improvements are associated with increases in mindfulness, and pain resilience and decreases in kinesiophobia. But these variables only appear to mediate the effects of the training with regard to disability.
Mindfulness has been well documented to improve the disability of chronic pain patients. It is not surprising that the ability to be resilient in the face of pain and the lowering the fear of moving with pain are also helpful. Chronic pain makes life miserable for the patients and the effectiveness of the mind-body physical activity program in improving physical ability is helpful to some extent in decreasing the disability resulting from the pain and reducing the patient’s suffering.
So, improve physical function in chronic pain patients with mind-body practice.
“The mind, emotions and attention play an important role in the experience of pain. In patients with chronic pain, stress, fear and depression can amplify the perception of pain. Mind-body approaches act to change a person’s mental or emotional state or utilise physical movement to train attention or produce mental relaxation.” – Craig Hassed
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Google+ https://plus.google.com/106784388191201299496/posts and on Twitter @MindfulResearch
Study Summary
Greenberg, J., Mace, R. A., Bannon, S. M., Kulich, R. J., & Vranceanu, A. M. (2021). Mind-Body Activity Program for Chronic Pain: Exploring Mechanisms of Improvement in Patient-Reported, Performance-Based and Ambulatory Physical Function. Journal of pain research, 14, 359–368. https://doi.org/10.2147/JPR.S298212
Abstract
Background
Improving physical function among patients with chronic pain is critical for reducing disability and healthcare costs. However, mechanisms underlying improvement in patient-reported, performance-based, and ambulatory physical function in chronic pain remain poorly understood.
Purpose
To explore psychosocial mediators of improvement in patient-reported, performance-based, and objective/accelerometer-measured physical function among participants in a mind-body activity program.
Methods
Individuals with chronic pain were randomized to one of two identical 10-week mind-body activity interventions aimed at improving physical function with (GetActive-Fitbit; N=41) or without (GetActive; N=41) a Fitbit device. They completed self-reported (WHODAS 2.0), performance-based (6-minute walk test), and objective (accelerometer-measured step-count) measures of physical function, as well as measures of kinesiophobia (Tampa Kinesiophobia Scale), mindfulness (CAMS-R), and pain resilience (Pain Resilience Scale) before and after the intervention. We conducted secondary data analyses to test mediation via mixed-effects modeline.
Results
Improvements in patient-reported physical function were fully and uniquely mediated by kinesiophobia (Completely Standardized Indirect Effect (CSIE)=.18; CI=0.08, 0.30; medium-large effect size), mindfulness (CSIE=−.14; CI=−25, −.05; medium effect size) and pain resilience (CSIE=−.07; CI=−.16, −.005; small-medium effect size). Improvements in performance-based physical function were mediated only by kinesiophobia (CSIE=−.11; CI=−23, −.008; medium effect size). No measures mediated improvements in objective (accelerometer measured) physical function.
Conclusion
Interventions aiming to improve patient-reported physical function in patients with chronic pain may benefit from skills that target kinesiophobia, mindfulness, and pain resilience, while those focused on improving performance-based physical function should target primarily kinesiophobia. More research is needed to understand mechanisms of improvement in objective, accelerometer-measured physical function.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7872894/