By John M. de Castro, Ph.D.
In today’s Research News article “Effects of Meditation and Yoga on Anxiety, Depression and Chronic Inflammation in Patients with Parkinson’s Disease: A Randomized Clinical Trial” (See summary below or view the full text of the study at: https://pmc.ncbi.nlm.nih.gov/articles/PMC11965853/ ) Kwok and colleagues studied the effects of meditation and yoga practice on the symptoms of Parkinson’s Disease. They found that these practices significantly relieved a wide variety of symptoms, including anxiety, depression, inflammation, movement problems, and improved quality of life.
Meditation and yoga relieve the symptoms of Parkinson’s disease.
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on the Contemplative Studies Blog http://contemplative-studies.org
Study Summary
Jojo Yan Yan Kwok, Lily Man Lee Chan, Charis Ann Lai, Philip Wing Lok Ho, Zoe Yuen-kiu Choi, Man Auyeung, Shirley Yin Yu Pang, Edmond Pui Hang Choi, Daniel Yee Tak Fong, Doris Sau Fung Yu, Chia-chin Lin, Richard Walker, Samuel Yeung Shan Wong, Rainbow Tin Hung Ho. Effects of Meditation and Yoga on Anxiety, Depression and Chronic Inflammation in Patients with Parkinson’s Disease: A Randomized Clinical Trial. Psychother Psychosom. 2025 Feb 28;94(2):101–118.
Abstract
Introduction
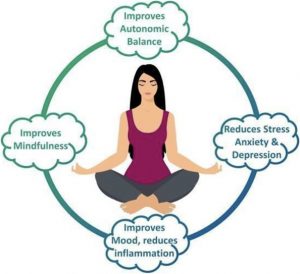
Clinical guidelines recommend a holistic approach to Parkinson’s disease (PD) care, yet randomized trials examining mindfulness-based interventions in this context are scarce. This study investigated the effects of two mindfulness practices – meditation and yoga – on biopsychosocial outcomes in PD patients, including anxiety symptoms, depressive symptoms, motor/nonmotor symptoms, health-related quality-of-life (HRQOL), mindfulness, and stress and inflammation biomarkers, compared to usual care.
Methods
159 participants with a clinical diagnosis of idiopathic PD and a Hoehn and Yahr stage of 1, 2, and 3, were randomized into meditation (n = 53), yoga (n = 52), and control (n = 54). Meditation and yoga were delivered in 90-min groups for 8 weeks. Primary outcomes included anxiety symptoms and depressive symptoms. Secondary outcomes included motor and nonmotor symptoms, HRQOL, mindfulness, and serum levels of interleukin-6, cortisol and TNF-alpha. Assessments were done at baseline (T0), 2 months (T1), and 6 months (T2). Linear mixed models were conducted following intention-to-treat principle.
Results
Compared to control, both meditation, and yoga groups had significant improvements in anxiety symptoms (meditation: mean difference [MD] = −1.36, 95% CI: −2.46 to−0.26; yoga: MD = −1.61, CI: −2.70 to −0.52), motor symptoms (meditation: MD = −5.35, CI: −8.61 to−2.09; yoga: MD = −6.59, CI: −9.82 to−3.36), HRQOL (meditation: MD = −2.01, CI: −3.41 to−0.62; yoga: MD = −1.45, CI: −2.83 to−0.08), and describing skills (meditation: MD = 0.97, CI: 0.04–1.89; yoga: MD = 0.92, CI: 0.01–1.84) at T1, and significant reductions in serum interleukin-6 levels (meditation: MD = −1.14, CI: −2.18 to−0.10; yoga: MD = −1.11, CI: −2.09 to−0.13) at T2. Only meditation significantly reduced depression (MD = −1.44, CI: −2.57 to−0.30) at T1 and sustained the motor and HRQOL improvements at T2.
Conclusion
Meditation and yoga significantly improved anxiety symptoms, chronic inflammation, motor symptoms, mindfulness-describing facet, and HRQOL in PD patients. Meditation provided additional benefits in reducing depressive symptoms and sustaining motor and HRQOL improvements.
 By John M. de Castro, Ph.D.
By John M. de Castro, Ph.D.