Improve Stress Responding, Health, and Well-Being with Qigong
By John M. de Castro, Ph.D.
“Qigong is an extraordinary tool for reducing the harmful effects of stress. The three pillars of qigong practice are body, breath, and mind. If your body is relaxed your breathing will slow down. When your breath is slow, you feel more centered, more calm, and more in touch with yourself” – Kenneth Cohen
Tai Chi and Qigong are ancient mindfulness practices involving slow prescribed movements. They are gentle and completely safe, can be used with the elderly and sickly, are inexpensive to administer, can be performed in groups or alone, at home or in a facility or even public park, and can be quickly learned. In addition, they can also be practiced in social groups without professional supervision. This can make it fun, improving the likelihood of long-term engagement in the practice.
Tai Chi and Qigong are both mindfulness practices and gentle exercises. They have been shown to be beneficial for the health and well-being of individuals of a variety of ages, but particularly the elderly. They also improve the symptoms of a variety of diseases. One way that these practices may improve health and well-being is by reducing stress. The studies of the benefits for health of Tai Chi and Qigong are accumulating and so it makes sense to take a moment to summarize what has been learned about the benefits of Qigong practice.
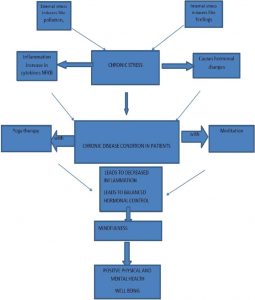
In today’s Research News article “Individual Stress Prevention through Qigong.” (See summary below or view the full text of the study at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7579037/ ) van Dam reviews and summarizes the published research studies of the effects of Qigong practice on stress. She reports that the published studies found that Qigong practice improves the cardiovascular system including a significant reduction in blood pressure and an increase in heartrate variability, an indicator of parasympathetic relaxation. It improves the respiratory system including increased lung capacity, oxygen intake and breathing patterns. It improves immune function and reduces inflammatory responses. It improves both psychological and physiological responses to stress. It improves sleep quality and reduces fatigue. It reduces depression and both acute and chronic anxiety.
These findings are remarkable and suggest that this gentle safe practice markedly improves the physical and mental well-being and health of the practitioners. Many of these benefits may result from the ability of Qigong practice to improve stress responding. Stress impairs health and well-being and Qigong practice appears to counteract these effects.
So, improve stress responding, health, and well-being with Qigong.
“Qi Gong helps you develop a crystal clear mind as you connect with the present moment, letting go of the stress of daily life and relaxing deeply.”- Nick Jankel
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Google+ https://plus.google.com/106784388191201299496/posts and on Twitter @MindfulResearch
Study Summary
van Dam K. (2020). Individual Stress Prevention through Qigong. International journal of environmental research and public health, 17(19), 7342. https://doi.org/10.3390/ijerph17197342
Abstract
Owing to work intensification and an accelerated pace of life in general, individuals in many Western countries are often overactivated and find it difficult to switch off. However, recovery from physiological and mental activation is critical to prevent stress symptoms and maintain one’s physiological and mental well-being. Extensive research evidence indicates that Qigong, a traditional Chinese movement practice for promoting health, provides an effective means to recover from work and off-work demands. The main objective of this paper is to offer a comprehensive, narrative review of the effects of Qigong and its core components. Attention is first paid to the outcomes of work and off-work demands and stress, and the role of recovery for individuals’ well-being. Then, Qigong and its components are explained, followed by the results of scientific research. Finally, limitations and implications for research and practiced are discussed.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7579037/