Reduce Dysfunctional Eating with Mindfulness
By John M. de Castro, Ph.D.
“The more you eat, the less flavor; the less you eat, the more flavor.” ~Chinese Proverb
Around 30 million people in the United States of all ages and genders suffer from an eating disorder: either anorexia nervosa, bulimia, or binge eating disorder. 95% of those who have eating disorders are between the ages of 12 and 26. Eating disorders are not just troubling psychological problems, they can be deadly, having the highest mortality rate of any mental illness. Two example of eating disorders are binge eating disorder (BED) and bulimia nervosa (BN). BED involves eating a large amount of food within a short time-period while experiencing a sense of loss of control over eating. BN involves binge-eating and purging (e.g., self-induced vomiting, compensatory exercise).
Eating disorders can be difficult to treat because eating is necessary and cannot be simply stopped as in smoking cessation or abstaining from drugs or alcohol. One must learn to eat appropriately not stop. So, it is important to find methods that can help prevent and treat eating disorders. Contemplative practices, mindfulness, and mindful eating have shown promise for treating eating disorders. It is not known however, if mindfulness training can improve dysregulated eating and in turn reduce the likelihood of eating disorders.
In today’s Research News article “Delivering Mindfulness-Based Interventions for Insomnia, Pain, and Dysfunctional Eating Through a Text Messaging App: Three Randomized Controlled Trials Investigating the Effectiveness and Mediating Mechanisms.” (See summary below or view the full text of the study at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9115660/ ) Li and colleagues recruited adults over the internet and provided mindfulness training through text messaging. They measured insomnia, pain, and dysregulated eating.
They found that mindfulness training compared to a wait-list control condition resulted in resulted in significant decreases in anxiety, depression, insomnia, pain, and dysregulated eating and these improvements were sustained 3 months after the end of training. They found a wide array of improvements from mindfulness training. Particularly important from the perspective of eating disorders were the findings of reductions in depression and dysregulated eating. This suggests that mindfulness training reduces the likelihood of the development of an eating disorder.
“When walking, walk. When eating, eat.” rashaski · Zen Proverb
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Twitter @MindfulResearch
Study Summary
Li AC, Wong KK, Chio FH, Mak WW, Poon LW. Delivering Mindfulness-Based Interventions for Insomnia, Pain, and Dysfunctional Eating Through a Text Messaging App: Three Randomized Controlled Trials Investigating the Effectiveness and Mediating Mechanisms. J Med Internet Res. 2022 May 3;24(5):e30073. doi: 10.2196/30073. PMID: 35503653; PMCID: PMC9115660.
Abstract
Background
Although text messaging has the potential to be the core intervention modality, it is often used as an adjunct only. To improve health and alleviate the distress related to insomnia, pain, and dysregulated eating of people living in urban areas, text messaging–based mindfulness-based interventions were designed and evaluated in 3 randomized controlled trials.
Objective
This study investigated the effectiveness and mediating mechanisms of text messaging–based mindfulness-based interventions for people with distress related to insomnia, pain, or dysregulated eating.
Methods
In these trials, 333, 235, and 351 participants were recruited online and randomized to intervention and wait-list control conditions for insomnia, pain, and dysregulated eating, respectively. Participants experienced 21 days of intervention through WhatsApp Messenger. Participants completed pre-, post-, 1-month follow-up, and 3-month follow-up self-report questionnaires online. The retention rates at postmeasurements were 83.2% (139/167), 77.1% (91/118), and 72.9% (129/177) for intervention groups of insomnia, pain, and dysregulated eating, respectively. Participants’ queries were answered by a study technician. Primary outcomes included insomnia severity, presleep arousal, pain intensity, pain acceptance, and eating behaviors. Secondary outcomes included mindfulness, depression, anxiety, mental well-being, and functional impairments. Mindfulness, dysfunctional beliefs and attitudes about sleep, pain catastrophizing, and reactivity to food cues were hypothesized to mediate the relationship between the intervention and outcomes.
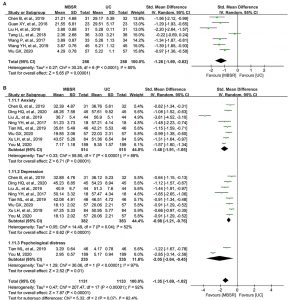
Results
For all 3 studies, the intervention groups showed significant improvement on most outcomes at 1-month follow-up compared to their respective wait-list control groups; some primary outcomes (eg, insomnia, pain, dysregulated eating indicators) and secondary outcomes (eg, depression, anxiety symptoms) were sustained at 3-month follow-up. Medium-to-large effect sizes were found at postassessments in most outcomes in all studies. In the intervention for insomnia, mediation analyses showed that dysfunctional beliefs and attitudes about sleep mediated the effect of the intervention on all primary outcomes and most secondary outcomes at both 1-month and 3-month follow-ups, whereas mindfulness mediated the intervention effect on presleep arousal at 1-month and 3-month follow-ups. In the intervention for pain, pain catastrophizing mediated the effect of intervention on pain intensity and functioning at both 1-month and 3-month follow-ups, whereas mindfulness only mediated the effect of intervention on anxiety and depressive symptoms. In the intervention for dysregulated eating, power of food mediated the effect of intervention on both uncontrolled and emotional eating at both 1-month and 3-month follow-ups and mindfulness was found to mediate the effect on depressive symptoms at both 1-month and 3-month follow-ups.
Conclusions
These 3 studies converged and provided empirical evidence that mindfulness-based interventions delivered through text messaging are effective in improving distress related to sleep, pain, and dysregulated eating. Text messaging has the potential to be a core intervention modality to improve various common health outcomes for people living a fast-paced lifestyle.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9115660/