Reduce Inflammatory Processes with Mindfulness
By John M. de Castro, Ph.D.
“Millions of people around the world already enjoy the health benefits of mind-body interventions like yoga or meditation, but what they perhaps don’t realize is that these benefits begin at a molecular level and can change the way our genetic code goes about its business. These activities are leaving what we call a molecular signature in our cells, which reverses the effect that stress or anxiety would have on the body by changing how our genes are expressed. Put simply, MBIs cause the brain to steer our DNA processes along a path which improves our wellbeing.” – Ivana Buric
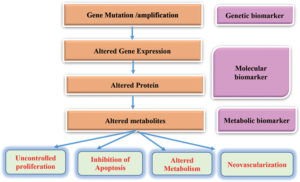
The immune system is designed to protect the body from threats like stress, infection, injury, and toxic chemicals. One of its tools is the Inflammatory response. This response works quite well for short-term infections and injuries. But when inflammation is protracted and becomes chronic, it can itself become a threat to health. It can produce autoimmune diseases such as colitis, Chron’s disease, arthritis, heart disease, increased cancer risk, lung disease, sleep disruption, gum disease, decreased bone health, psoriasis, and depression. Needless to say, chronic inflammation can create major health problems. Indeed, the presence of chronic inflammation is associated with reduced longevity. So, it is important for health to control the inflammatory response, allowing it to do its job in fighting off infection but reducing its activity when no external threat is apparent.
Of course, it is far better to prevent chronic inflammation in the first place than to treat it later. Mind-body techniques such as yoga, Tai Chi and meditation have been shown to adaptively reduce the inflammatory response. In today’s Research News article “Effects of Mind-Body Training on Cytokines and Their Interactions with Catecholamines.” (See summary below or view the full text of the study at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5561407/ ), Jang and colleagues recruited healthy adult Mind-Body Training (MBT) practitioners and a group of healthy adult non-practitioners. MBT consists of a combination of mindful movements, breathing exercises, and meditation. The recruited practitioners engaged in MBT on average for about an hour three or four times per week. Blood samples from all participants were drawn and assayed for cytokines, including TNF-Alpha, IL-6, IL-10, and IFN-Gamma, and the catecholamines, Norepinephrine, Epinephrine, and Dopamine.
They found that the Mind-Body Training (MBT) group had significantly higher levels of the anti-inflammatory cytokine, IL-10. Levels of the pro-inflammatory cytokines were lower in the MBT groups but the differences were not significant. In addition, they found that the higher the levels of IL-10, the higher the levels of the catecholamine ratios of Norepinephrine/Epinephrine and Dopamine/Epinephrine. Hence, MBT practice appears to be associated with decreases in inflammatory processes. In addition, high catecholamine ratios are associated with decreased stress levels, suggesting that the high IL-10 levels observed in the MBT group are associated with lower levels of stress.
The study did not actively manipulate MBT practice, so no conclusions about causation can be reached. The results, however, support the hypothesis that Mind-Body Training (MBT) is associated with decreased inflammatory responses and stress levels. Other research has shown that mindfulness practice can reduce inflammation and stress. So, it is reasonable to conclude that the present results were due to MBT practice. Since, chronic inflammation is detrimental to the health of the individual, the results suggest that MBT practice would help to improve or maintain the health and longevity of the individual.
So, reduce inflammatory processes with mindfulness.
“Chronic inflammation is associated with increased risk for psychiatric disorders, autoimmune conditions such as asthma and arthritis, cardiovascular disease, neurodegenerative disease and some types of cancer. But . . . mind-body interventions might help reduce the risk for inflammation-related disorders. And not just psychological ones, but even the physical ones like asthma or arthritis.” – Jo Marchant
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Google+ https://plus.google.com/106784388191201299496/posts and on Twitter @MindfulResearch
Study Summary
Jang, J. H., Park, H. Y., Lee, U. S., Lee, K.-J., & Kang, D.-H. (2017). Effects of Mind-Body Training on Cytokines and Their Interactions with Catecholamines. Psychiatry Investigation, 14(4), 483–490. http://doi.org/10.4306/pi.2017.14.4.483
Abstract
Objective
Mind-body training (MBT) may control reactions to stress and regulate the nervous and immune systems. The present study was designed to assess the effects of MBT on plasma cytokines and their interactions with catecholamines.
Methods
The study group consisted of 80 subjects who practice MBT and a control group of 62 healthy subjects. Plasma catecholamine (norepinephrine, NE; epinephrine, E; and dopamine, DA) and cytokine (TNF-alpha, IL-6, IFN-gamma, and IL-10) levels were measured, and the differences between the MBT and control groups and the interactions of cytokines with catecholamines were investigated.
Results
A significant increase in IL-10+IFN-gamma was found in females of the MBT group compared with controls. Also, a significant increase of IL-10 (anti-inflammatory cytokine) in the MBT group was shown in a specific condition in which TNF-alpha and IL-6 (pro-inflammatory cytokines) are almost absent (≤1 ng/L) compared with controls. In the MBT group, significant positive correlations were found between IL-10 and the NE/E ratio and between IL-10 and the DA/E ratio, whereas the control group did not show any such correlations.
Conclusion
MBT may increase IL-10, under specific conditions such as a decrease of pro-inflammatory cytokines or E, which may regulate the stress response and possibly contribute to effective and beneficial interactions between the nervous and immune systems.