Reduce Age-Related Decline in the Brain with Mindfulness
By John M. de Castro, Ph.D.
“Long-term engagement in mindfulness meditation may enhance cognitive performance in older adults, and that with persistent practice, these benefits may be sustained. That’s great news for the millions of aging adults working to combat the negative effects of aging on the brain.” – B Grace Bullock
The aging process involves a systematic progressive decline in every system in the body, the brain included. This includes our mental abilities which decline with age including impairments in memory, attention, and problem-solving ability. It is inevitable and cannot be avoided. Using modern neuroimaging techniques, scientists have been able to view the changes that occur in the nervous system with aging. In addition, they have been able to investigate various techniques that might slow the process of neurodegeneration that accompanies normal aging. They’ve found that mindfulness practices reduce the deterioration of the brain that occurs with aging restraining the loss of neural tissue. Indeed, the brains of practitioners of meditation and yoga have been found to degenerate less with aging than non-practitioners.
In today’s Research News article “Default Mode Network, Meditation, and Age-Associated Brain Changes: What Can We Learn from the Impact of Mental Training on Well-Being as a Psychotherapeutic Approach?” (See summary below or view the full text of the study at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6466873/), Ramírez-Barrantes and colleagues review and summarize the research on the effects of meditation practice on brain function and aging focusing primarily on the Default Mode Network (DMN). It is composed of interconnected brain regions including the medial prefrontal cortex, posterior cingulate cortex, precuneus, inferior parietal lobule, and inferolateral temporal cortex. It is active when the mind is wandering and when the individual is involved in self-referential thinking.
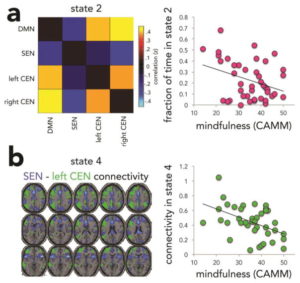
Increased activation and functional connectivity of the Default Mode Network (DMN) are associated with the cognitive decline with aging. This makes sense as increased mind wandering would interfere with the attentional focus needed for high level thinking. Mindfulness practices such as meditation and yoga have been shown to both reduce the cognitive decline with aging and also to decrease the activation and functional connectivity of the DMN. This suggests that mindfulness practices may help prevent the cognitive decline in aging in part by reducing the activity of the DMN.
Ramírez-Barrantes and colleagues propose that age-related cognitive decline may be slowed or prevented by engaging in mindfulness practices that reduce the activity of the Default Mode Network (DMN). This would reduce mind wandering and improve attention focus resulting in a greater ability to engage in high level thinking. Much more research is needed to explore this interesting possibility.
So, reduce age-related decline in the brain with mindfulness.
“experienced meditators have higher concentrations of tissue in brain regions most depleted by aging. This suggests that meditation practice may help to minimize brain age and protect against age-related decline.” – Matt Caron
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Google+ https://plus.google.com/106784388191201299496/posts and on Twitter @MindfulResearch
Study Summary
Ramírez-Barrantes, R., Arancibia, M., Stojanova, J., Aspé-Sánchez, M., Córdova, C., & Henríquez-Ch, R. A. (2019). Default Mode Network, Meditation, and Age-Associated Brain Changes: What Can We Learn from the Impact of Mental Training on Well-Being as a Psychotherapeutic Approach?. Neural Plasticity, 2019, 7067592. doi:10.1155/2019/7067592
Abstract
Aging is a physiological process accompanied by cognitive decline, principally in memory and executive functions. Alterations in the connectivity of the default mode network (DMN) have been found to participate in cognitive decline, as well as in several neurocognitive disorders. The DMN has antisynchronic activity with attentional networks (task-positive networks (TPN)), which are critical to executive function and memory. Findings pointing to the regulation of the DMN via activation of TPN suggest that it can be used as a strategy for neuroprotection. Meditation is a noninvasive and nonpharmacological technique proven to increase meta-awareness, a cognitive ability which involves the control of both networks. In this review, we discuss the possibility of facilitating healthy aging through the regulation of networks through meditation. We propose that by practicing specific types of meditation, cognitive decline could be slowed, promoting a healthy lifestyle, which may enhance the quality of life for the elderly.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6466873/