Reduce the Symptoms of Schizophrenia with Mind-Body Practices
By John M. de Castro, Ph.D.
“Research shows that some mindfulness-based interventions for psychotic symptoms can afford people a greater acceptance and insight into their experiences. They can also reduce the symptoms of anxiety and depression which often accompany, and may exacerbate, psychotic disorders.” – Adrianna Mendrek
Schizophrenia is the most common form of psychosis. Its effects about 1% of the population worldwide. It appears to be highly heritable and involves changes in the brain. It is characterized by both positive and negative symptoms. Positive symptoms include hallucinations; seeing and, in some cases, feeling, smelling or tasting things that aren’t there, or delusions; unshakable beliefs that, when examined rationally, are obviously untrue. Negative symptoms include a reduced ability to function normally, neglect of personal hygiene, lack of emotion, blank facial expressions, speaking in a monotone, loss of interest in everyday activities, social withdrawal, an inability to experience pleasure, and a lack of insight into their symptoms. The symptoms of schizophrenia usually do not appear until late adolescence or early adulthood.
Schizophrenia is very difficult to treat with psychotherapy and is usually treated with antipsychotic drugs. These drugs, however, are not always effective, sometimes lose effectiveness, and can have some difficult side effects. Mindfulness training has been shown to be beneficial for a variety of mental health problems, including psychosis. Mindfulness has also been shown to associated with lower symptom severity of schizophrenia. Also, there is accumulating research that mindfulness and yoga practices may be beneficial for patients with major mental illnesses. Tai Chi and Qigong practices have also been shown to improve the symptoms of schizophrenia. The evidence is accumulating. So, it makes sense to step back and summarize what has been learned about mind-body practices as treatments for schizophrenia.
In today’s Research News article “Effects of Mind-Body Exercises on Schizophrenia: A Systematic Review With Meta-Analysis.” (See summary below or view the full text of the study at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7457019/ ) Wei and colleagues review, summarize and perform a meta-analysis of the published controlled research studies of the effectiveness of mind-body practices to improve the symptoms of schizophrenia. They included Tai Chi, Qigong, yoga, and other mindful movement practices. They identified 13 studies (11 randomized controlled trials) employing a total of 1159 patients with schizophrenia.
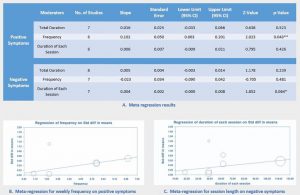
They report that the published studies found that mind-body practices produced significant improvements of both the positive and negative symptoms of schizophrenia and also depression. In addition, the greater the number of weekly mind-body sessions the greater the improvement in the positive symptoms and the greater the duration of the mind-body sessions the greater the improvements in the negative symptoms.
These results are impressive as schizophrenia is difficult to treat. But the results show that mind-body practices are safe and effective treatments that improve not only the positive and negative symptoms of schizophrenia but also the frequently co-occurring depression. There also appears to be a dose response effect such that the greater the frequency and duration of mind-body practices the greater the benefits. This suggests that mind-body practices should be recommended as a part of the treatment for schizophrenia.
So, reduce the symptoms of schizophrenia with mind-body practices.
“yoga therapy is of particular benefit for those with schizophrenia . . in lessening state anxiety and increasing subjective wellbeing, while also reducing both positive and negative symptoms and improving quality of life.” – Minded Institute
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Google+ https://plus.google.com/106784388191201299496/posts and on Twitter @MindfulResearch
Study Summary
Wei, G. X., Yang, L., Imm, K., Loprinzi, P. D., Smith, L., Zhang, X., & Yu, Q. (2020). Effects of Mind-Body Exercises on Schizophrenia: A Systematic Review With Meta-Analysis. Frontiers in psychiatry, 11, 819. https://doi.org/10.3389/fpsyt.2020.00819
Abstract
Background
Mind–body exercises (MBEs) have been widely accepted as a complementary therapy for the patients with low exercise tolerance. Currently, the number of experimental studies investigating the effect of MBEs for improving symptoms in people with schizophrenia is increasing. However, results are inconsistent.
Methods
We systematically reviewed and meta-analyzed the effects of mind–body exercises on schizophrenia. Seven electronic databases (Pubmed, Web of Science, PsycINFO, Embase, Cochrane Central Register of Controlled Trials [CENTRAL], CNKI and Wangfang) were screened through October 2019 and risks of bias of included studies were assessed in Review Manager 5.3.
Results
Meta-analysis on 13 studies with 1,159 patients showed moderately significant effects in favor of mind–body exercise intervention to improve positive symptoms (SMD = 0.31; 95% CI 0.01 to 0.60; p = 0.04), negative symptoms (SMD = 0.37; 95% CI 0.14 to 0.60; p = 0.002), and depression (SMD = 0.88; 95% CI 0.63 to 1.13; p<0.00001). Meta-regression analysis revealed that the improvement in positive symptoms was positively associated with the frequency of intervention (p = 0.04), while a marginally significant correlation was observed between the improved negative symptoms and duration of each session (p = 0.06).
Conclusions
This meta-analysis supports the therapeutic effects of MBEs to aid in the treatment of schizophrenia. Further studies need to incorporate rigorous design and large sample size to identify the optimal type and dose of mind–body exercise to inform clinical practices on MBEs’ recommendations for the management of schizophrenia symptoms.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7457019/