Improve Brain Processing of Awareness and Emotions with Mindfulness
By John M. de Castro, Ph.D.
“Evidence suggests that particular areas of the brain may either shrink or grow in response to regular mindfulness practice.” – Meera Joshi
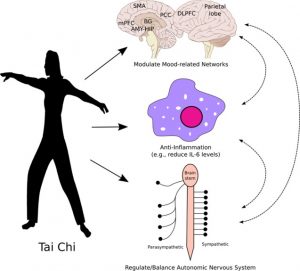
There has accumulated a large amount of research demonstrating that meditation practice has significant benefits for psychological, physical, and spiritual wellbeing. One way that meditation practices may produce these benefits is by altering the brain. The nervous system is a dynamic entity, constantly changing and adapting to the environment. It will change size, activity, and connectivity in response to experience. These changes in the brain are called neuroplasticity.
Neuroscience has established that contemplative practices produce neuroplastic changes in widespread areas of the nervous system. In other words, mindfulness practices appears to mold and change the brain, producing psychological, physical, and spiritual benefits. One mindfulness therapeutic technique, Mindfulness-Based Stress Reduction (MBSR), has been commonly applied to the treatment of multiple physical and psychological conditions. The MBSR practice consists of discussion, meditation, yoga, and body scan practices. It is important to understand what are the exact changes in the brain that are produced by the MBSR training.
In today’s Research News article “Alterations of Regional Homogeneity and Functional Connectivity Following Short-Term Mindfulness Meditation in Healthy Volunteers.” (See summary below or view the full text of the study at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6813410/), Xiao and colleagues recruited meditation naive healthy adults who were participating in an MBSR training and a matched group of no-treatment control participants. The MBSR program met for 2 hours once a week for 8 weeks along with daily home practice. They were measured before and after training for mindfulness and positive and negative emotions. In addition, the participants’ brains were scanned with a functional magnetic resonance imaging (fMRI) technique.
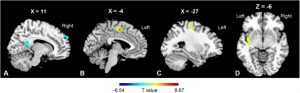
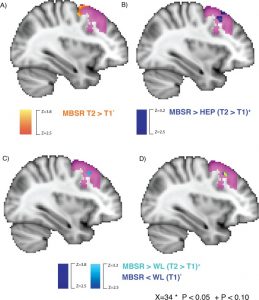
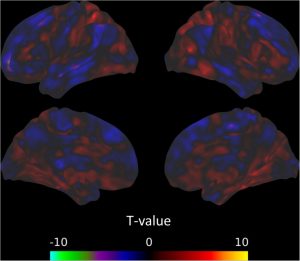
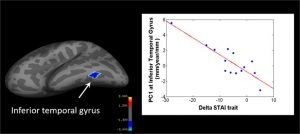
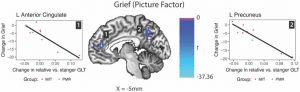
They found that in comparison to baseline and the no-treatment controls, the participants in the Mindfulness-Based Stress Reduction (MBSR) training had significant increases in mindfulness and significant decreases in negative emotions. They also found that following MBSR training there were significant increases in the synchronization of activities in the parietal lobe and significant decreases in the synchronization of activities in the posterior cingulate cortex, precuneus, and cuneus, and increased functional connectivity in the superior parietal lobule and postcentral gyrus and the median cingulate cortex, insula and precentral gyrus.
The findings that Mindfulness-Based Stress Reduction (MBSR) training increases mindfulness and decreases negative emotions and affects brain structures and connectivity are well established by other studies. The parietal lobe is known to be involved in attentional and executive control brain networks. So, the findings that its’ activities synchronizations were increased by MBSR training are also not surprising, suggesting that the training improves attention. Likewise, and the posterior cingulate cortex is associated with what’s called the default mode network which is associated with mind wandering and discursive and internalized thinking. So, the findings that its’ activity synchronizations were decreased by MBSR training are also not surprising, suggesting that the training reduces mind wandering.
In addition, the findings that Mindfulness-Based Stress Reduction (MBSR) training increases functional connectivity of the median cingulate cortex and insula would be expected as these structures are involved in interoceptive awareness, suggesting that MBSR training heightens the awareness of the practitioner’s internal state. Finally, the findings that MBSR training increases functional connectivity of the precentral and postcentral gyrus would be expected as these structures are involved in coordination of tactile and motor information, suggesting that MBSR training heightens the bodily awareness, another component of mindfulness.
The findings, then, of the present study are compatible with prior findings of the effects of Mindfulness-Based Stress Reduction (MBSR) training on the practitioners’ psychological states and the brain systems underlying these states. This helps to present a clearer picture of the impact of mindfulness training on the individuals psychological processes and their underlying neural substrates. MBSR training is a combination of meditation, yoga, body scan, and experience sharing. It remains for future research to delineate which components or combinations of components may or may not be responsible for each of these effects.
So, improve brain processing of awareness and emotions with mindfulness.
“The impact that mindfulness exerts on our brain is borne from routine: a slow, steady, and consistent reckoning of our realities, and the ability to take a step back, become more aware, more accepting, less judgmental, and less reactive. . . mindfulness over time can make the brain, and thus, us, more efficient regulators, with a penchant for pausing to respond to our worlds instead of mindlessly reacting.” – Jennifer Wolkin
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Google+ https://plus.google.com/106784388191201299496/posts and on Twitter @MindfulResearch
Study Summary
Xiao, Q., Zhao, X., Bi, G., Wu, L., Zhang, H., Liu, R., … Chen, Z. (2019). Alterations of Regional Homogeneity and Functional Connectivity Following Short-Term Mindfulness Meditation in Healthy Volunteers. Frontiers in human neuroscience, 13, 376. doi:10.3389/fnhum.2019.00376
Abstract
Mindfulness is described as the non-judgmental awareness of experiences in the present moment. The sustained practice of mindfulness may also have beneficial effects on an individual’s well-being. For instance, mindfulness meditation is an effective approach for improving emotion regulation. Specifically, the early stage of mindfulness meditation training enhances emotional monitoring systems related to attention regulation and executive function. Reduced activity in the default mode network (DMN) would probably be observed corresponding to the attenuated mind wandering. In the present study, we hypothesized that alterations in functional activity in the frontal-parietal cortex and DMN may be induced by short-term mindfulness meditation. In this study, before and after 8 weeks of weekly Mindfulness-Based Stress Reduction (MBSR) training, healthy participants were evaluated using a mindfulness questionnaire and an affect schedule, as well as via resting-state functional magnetic resonance imaging. Sixteen right-handed non-meditators were enrolled. Another 16 demographically matched healthy adults without any meditation experience were recruited as controls. Pre- and post-MBSR assessments were compared. Increased regional homogeneity in the right superior parietal lobule and left postcentral gyrus (PoCG), as well as altered functional connectivity in PoCG-related networks, were observed post-MBSR. The mindfulness questionnaire scores also improved and negative affect was significantly decreased after MBSR. Together with reduced involvement of the posterior brain, our results suggest a tendency toward stronger involvement of the parietal cortex in mindfulness beginners. This study provides novel evidence regarding the optimization of emotional processing with short-term mindfulness meditation.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6813410/