Improve Athletes’ Psychological Well-Being and Flow with Mindfulness
By John M. de Castro, Ph.D.
“You have to be able to center yourself, to let all of your emotions go. Don’t forget that you play with your soul as well as your body.” Kareem Abdul-Jabbar
Athletic performance requires the harmony of mind and body. Excellence is in part physical and in part psychological. That is why an entire profession of sports psychology has developed. “In sport psychology, competitive athletes are taught psychological strategies to better cope with a number of demanding challenges related to psychological functioning.” They use a number of techniques to enhance performance including mindfulness training. It has been shown to improve attention and concentration and emotion regulation and reduces anxiety and worry and rumination, and the physiological and psychological responses to stress. As a result, mindfulness training has been employed by athletes and even by entire teams to enhance their performance.
Flow refers to a state of mind that is characterized by a complete absorption with the task at hand, often resulting in enhanced skilled performance. The flow state underlies the athletes’ feelings and thoughts when they recall the best performances of their careers. It is obvious that the notion of flow and mindfulness have great similarity. There is little known, however, about the relationship between mindfulness and flow in athletes.
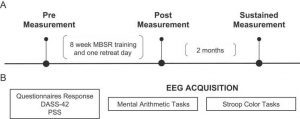
In today’s Research News article “Effects of “Mindfulness Acceptance Insight Commitment” Training on Flow State and Mental Health of College Swimmers: A Randomized Controlled Experimental Study.” (See summary below or view the full text of the study at: https://www.frontiersin.org/articles/10.3389/fpsyg.2022.799103/full?utm_source=F-AAE&utm_medium=EMLF&utm_campaign=MRK_1896364_a0P58000000G0YfEAK_Psycho_20220705_arts_A&id_mc=312338674&utm_source=sfmc&utm_medium=email&utm_campaign=Article+Alerts+V4.1-Frontiers&utm_term=%%%3d+++++++REDIRECTTO(+++++CONCAT(%27http%3a%2f%2fjournal.frontiersin.org%2farticle%2f%27%2c+TreatAsContent(field(%40article%2c+%27DOI__c%27))%2c+%27%2ffull%3futm_source%3dF-AAE%26utm_medium%3dEMLF%26utm_campaign%3dMRK_%27%2c+TreatAsContent(JobID)%2c+%27_%27%2c+TreatAsContent(%40FieldId)%2c+%27_%27%2c+TreatAsContent(Substring(Replace(Field(%40field%2c+%27Name%27)%2c+%27+%27% ) Ning and colleagues recruited college swimming athletes and randomly assigned them to either no-treatment or to receive 7 weekly 90 minute mindfulness acceptance insight commitment training sessions, They were measured before and after training and 10 weeks late for mindfulness, flow, competitive anxiety, mood, and training and competition satisfaction.
They found that in comparison to baseline and the no-treatment control, the swimmers who received mindfulness training had significant increases in mindfulness and flow and significantly lower levels of anxiety and depression that were maintained 10 weeks later. Increased levels of flow have been associated with better athletic performance. This suggests that the mindfulness training may produce better swimming performance.
So, mindfulness improves athletes’ psychological well-being and flow.
“Champions aren’t made in gyms. Champions are made from something they have deep inside of them; a desire, a dream, a vision.” Muhammad Ali
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Twitter @MindfulResearch
Study Summary
Ning J-h, Hao Q-w and Huang D-c (2022) Effects of “Mindfulness Acceptance Insight Commitment” Training on Flow State and Mental Health of College Swimmers: A Randomized Controlled Experimental Study. Front. Psychol. 13:799103. doi: 10.3389/fpsyg.2022.799103
This research explores the intervention effect of the mindfulness acceptance insight commitment (MAIC) training program on the mindfulness level, flow state, and mental health of college swimmers. A sample of 47 college swimmers from a regular university was recruited and randomly divided into two groups before the intervention. Independent variables between groups are psychological training mode (MAIC training/no training), and the independent variable within group was time (pre-test, post-test, and continuity test). The dependent variables are mindfulness level, flow state, and mental health (anxiety, depression, training, and competition satisfaction). Results show that after the intervention of MAIC training, the mindfulness level of athletes’ flow state has been significantly improved, whereas anxiety and depression significantly decreased. In addition, the satisfaction with training and competition significantly improved. In the continuous stage after the intervention, the mindfulness level, flow state, and mental health of athletes are still significantly higher than those in the pre-test. The comparison of the post-test and continuity test show no significant differences in the mindfulness level, flow state, depression, and training and competition satisfaction of athletes. Still, the anxiety level shows an upward trend with a significant difference. This study demonstrates that the MAIC mindfulness training program can significantly improve the mindfulness level, flow state, anxiety, depression, and training and competition satisfaction of college swimmers with a good continuity effect. Thus, the athletes’ sports experience can be improved, and good psychological benefits can be attained.