Mindfulness Training Alters the Brain to Improve Internally Oriented Attention
By John M. de Castro, Ph.D.
“Regular practice of mindfulness can help you grow a wiser, more connected, and stress-proof brain.” – Melanie Greenberg
There has accumulated a large amount of research demonstrating that meditation practice has significant benefits for psychological, physical, and spiritual wellbeing. One way that meditation practices may produce these benefits is by altering the brain. Meditation practice appears to mold and change the brain structures and connectivity, producing psychological, physical, and spiritual benefits, especially mindfulness.
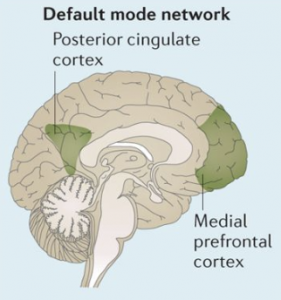
Meditation practice results in a shift in mental processing. It produces a reduction of mind wandering and self-referential thinking and an increase in attention and higher-level thinking. The neural system that underlie mind wandering is termed the Default Mode Network (DMN) and consists in a set of brain structures including medial prefrontal cortex, posterior cingulate, lateral temporal cortex and the hippocampus. The neural system that underlies executive functions such as attention and higher-level thinking is termed the Central Executive Network (CEN) and includes the dorsolateral prefrontal cortex, posterior parietal cortex, and cingulate cortex. The salience network has been shown to direct attention to significant aspects of the environment. Hence the shift in thought process may well be associated with changes in the relationship of these systems.
The evidence of the effects of mindfulness practices on the Default Mode Network (DMN) and the Salience Network has been accumulating. So, it makes sense to summarize what has been learned. In today’s Research News article “Meta-analytic evidence that mindfulness training alters resting state default mode network connectivity.” (See summary below or view the full text of the study at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9293892/ ) Rahrig and colleagues review, summarize, and perform a meta-analysis of the published research on the effects of mindfulness training on brain systems.
They identified 12 published research studies. They report that the research studies found that mindfulness training produced increased functional connectivity between the dorsal anterior cingulate cortex a component of the salience network and the posterior cingulate cortex a component of the default mode network. This suggests that mindfulness training increases the attention to significant aspects of internal processes. It can be hypothesized that this results in an internal attention to the internal mental processes of the mind.
“How we pay attention to the present moment largely determines the character of our experience, and therefore, the quality of our lives.” – Sam Harris
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Twitter @MindfulResearch
Study Summary
Rahrig H, Vago DR, Passarelli MA, Auten A, Lynn NA, Brown KW. Meta-analytic evidence that mindfulness training alters resting state default mode network connectivity. Sci Rep. 2022 Jul 18;12(1):12260. doi: 10.1038/s41598-022-15195-6. PMID: 35851275; PMCID: PMC9293892.
Abstract
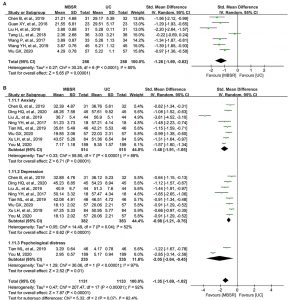
This meta-analysis sought to expand upon neurobiological models of mindfulness through investigation of inherent brain network connectivity outcomes, indexed via resting state functional connectivity (rsFC). We conducted a systematic review and meta-analysis of rsFC as an outcome of mindfulness training (MT) relative to control, with the hypothesis that MT would increase cross-network connectivity between nodes of the Default Mode Network (DMN), Salience Network (SN), and Frontoparietal Control Network (FPCN) as a mechanism of internally-oriented attentional control. Texts were identified from the databases: MEDLINE/PubMed, ERIC, PSYCINFO, ProQuest, Scopus, and Web of Sciences; and were screened for inclusion based on experimental/quasi-experimental trial design and use of mindfulness-based training interventions. RsFC effects were extracted from twelve studies (mindfulness n = 226; control n = 204). Voxel-based meta-analysis revealed significantly greater rsFC (MT > control) between the left middle cingulate (Hedge’s g = .234, p = 0.0288, I2 = 15.87), located within the SN, and the posterior cingulate cortex, a focal hub of the DMN. Egger’s test for publication bias was nonsignificant, bias = 2.17, p = 0.162. In support of our hypothesis, results suggest that MT targets internetwork (SN-DMN) connectivity implicated in the flexible control of internally-oriented attention.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9293892/