Alter the Genes for Better Health with Meditation
By John M. de Castro, Ph.D.
“meditation practices seem . . . promote endocrinal, neuronal, and behavioral functions. This suggests that the achievement of a state of inner silence through the practice of meditation can prevent or reverse the detrimental effects of a stressful environment.“ – Sabrina Venditti
Over the last several decades, research and anecdotal experiences have accumulated an impressive evidential case that the development of mindfulness has positive benefits for the individual’s mental, physical, and spiritual life. Mindfulness appears to be beneficial both for healthy people and for people suffering from a myriad of illnesses. It appears to be beneficial across ages, from children to the elderly. And it appears to be beneficial across genders, personalities, race, and ethnicity. The breadth and depth of benefits is unprecedented.
Meditation practice has been shown to improve health and longevity. One way it appears to act is by altering the genes which govern cellular processes in our bodies. The genes dictate all of the chemical processes in our bodies including immune and inflammatory responses. The ability of outside influences to affect gene expression is known as epigenetics. Hence, it is important to study the epigenetic alterations in gene expressions produced by meditation practice to determine if these effects are the intermediary between meditation and health.
In today’s Research News article “Transcriptomics of Long-Term Meditation Practice: Evidence for Prevention or Reversal of Stress Effects Harmful to Health.” (See summary below or view the full text of the study at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8001870/ ) Wenuganen and colleagues recruited older (> 60 years of age) healthy adult experienced practitioners of Transcendental Meditation and matched non-practitioners. Blood was drawn and analyzed for gene expression with microarrays and polymerase chain reaction.
They found that the genes of the Transcendental Meditation practitioners were in general significantly downregulated (lower expression) than the non-practitioners. “Sixty-two genes were related to hematologic diseases, 26 to coronary artery disease, 34 to diabetes complications, 49 to inflammation, and 64 to CVD. All these disease-related genes were downregulated in the TM group relative to the control group.” The genes found to have lower expression in the Transcendental Meditation practitioners were related to inflammatory responses and suppressed energy efficiency, while those upregulated (higher expression) were related to immune system function.
These epigenetic findings suggest that Transcendental Meditation practice over years of practice improve the immune system and energy efficiency while reducing inflammation in older individuals. These epigenetic changes suggest that Transcendental Meditation practice improves the physiology’s ability to maintain health by being better prepared to respond to disease and stress. This suggests a mechanism by which meditation practice improves health and longevity.
So, alter the genes for better health with meditation.
“meditation, yoga, and Tai Chi . . . all seem to have a beneficial effect on the expression of a slew of different genes. And, as you might expect, the affected genes are generally those involved in stress and inflammation.” – Alice Walton
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are a
Alter the Genes for Better Health with Meditation
By John M. de Castro, Ph.D.
“meditation practices seem . . . promote endocrinal, neuronal, and behavioral functions. This suggests that the achievement of a state of inner silence through the practice of meditation can prevent or reverse the detrimental effects of a stressful environment.“ – Sabrina Venditti
Over the last several decades, research and anecdotal experiences have accumulated an impressive evidential case that the development of mindfulness has positive benefits for the individual’s mental, physical, and spiritual life. Mindfulness appears to be beneficial both for healthy people and for people suffering from a myriad of illnesses. It appears to be beneficial across ages, from children to the elderly. And it appears to be beneficial across genders, personalities, race, and ethnicity. The breadth and depth of benefits is unprecedented.
Meditation practice has been shown to improve health and longevity. One way it appears to act is by altering the genes which govern cellular processes in our bodies. The genes dictate all of the chemical processes in our bodies including immune and inflammatory responses. The ability of outside influences to affect gene expression is known as epigenetics. Hence, it is important to study the epigenetic alterations in gene expressions produced by meditation practice to determine if these effects are the intermediary between meditation and health.
In today’s Research News article “Transcriptomics of Long-Term Meditation Practice: Evidence for Prevention or Reversal of Stress Effects Harmful to Health.” (See summary below or view the full text of the study at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8001870/ ) Wenuganen and colleagues recruited older (> 60 years of age) healthy adult experienced practitioners of Transcendental Meditation and matched non-practitioners. Blood was drawn and analyzed for gene expression with microarrays and polymerase chain reaction.
They found that the genes of the Transcendental Meditation practitioners were in general significantly downregulated (lower expression) than the non-practitioners. “Sixty-two genes were related to hematologic diseases, 26 to coronary artery disease, 34 to diabetes complications, 49 to inflammation, and 64 to CVD. All these disease-related genes were downregulated in the TM group relative to the control group.” The genes found to have lower expression in the Transcendental Meditation practitioners were related to inflammatory responses and suppressed energy efficiency, while those upregulated (higher expression) were related to immune system function.
These epigenetic findings suggest that Transcendental Meditation practice over years of practice improve the immune system and energy efficiency while reducing inflammation in older individuals. These epigenetic changes suggest that Transcendental Meditation practice improves the physiology’s ability to maintain health by being better prepared to respond to disease and stress. This suggests a mechanism by which meditation practice improves health and longevity.
So, alter the genes for better health with meditation.
“meditation, yoga, and Tai Chi . . . all seem to have a beneficial effect on the expression of a slew of different genes. And, as you might expect, the affected genes are generally those involved in stress and inflammation.” – Alice Walton
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are available at the Contemplative Studies Blog http://contemplative-studies.org/wp/
They are also available on Google+ https://plus.google.com/106784388191201299496/posts and on Twitter @MindfulResearch
Study Summary
Wenuganen, S., Walton, K. G., Katta, S., Dalgard, C. L., Sukumar, G., Starr, J., Travis, F. T., Wallace, R. K., Morehead, P., Lonsdorf, N. K., Srivastava, M., & Fagan, J. (2021). Transcriptomics of Long-Term Meditation Practice: Evidence for Prevention or Reversal of Stress Effects Harmful to Health. Medicina (Kaunas, Lithuania), 57(3), 218. https://doi.org/10.3390/medicina57030218
Abstract
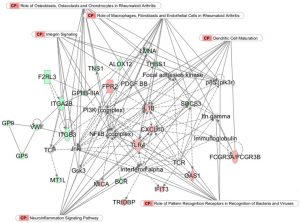
Background and Objectives: Stress can overload adaptive mechanisms, leading to epigenetic effects harmful to health. Research on the reversal of these effects is in its infancy. Early results suggest some meditation techniques have health benefits that grow with repeated practice. This study focused on possible transcriptomic effects of 38 years of twice-daily Transcendental Meditation® (TM®) practice. Materials and Methods: First, using Illumina® BeadChip microarray technology, differences in global gene expression in peripheral blood mononuclear cells (PBMCs) were sought between healthy practitioners and tightly matched controls (n = 12, age 65). Second, these microarray results were verified on a subset of genes using quantitative polymerase chain reaction (qPCR) and were validated using qPCR in larger TM and control groups (n = 45, age 63). Bioinformatics investigation employed Ingenuity® Pathway Analysis (IPA®), DAVID, Genomatix, and R packages. Results: The 200 genes and loci found to meet strict criteria for differential expression in the microarray experiment showed contrasting patterns of expression that distinguished the two groups. Differential expression relating to immune function and energy efficiency were most apparent. In the TM group, relative to the control, all 49 genes associated with inflammation were downregulated, while genes associated with antiviral and antibody components of the defense response were upregulated. The largest expression differences were shown by six genes related to erythrocyte function that appeared to reflect a condition of lower energy efficiency in the control group. Results supporting these gene expression differences were obtained with qPCR-measured expression both in the well-matched microarray groups and in the larger, less well-matched groups. Conclusions: These findings are consistent with predictions based on results from earlier randomized trials of meditation and may provide evidence for stress-related molecular mechanisms underlying reductions in anxiety, post-traumatic stress disorder (PTSD), cardiovascular disease (CVD), and other chronic disorders and diseases.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8001870/
re also available on Google+ https://plus.google.com/106784388191201299496/posts and on Twitter @MindfulResearch
Study Summary
Wenuganen, S., Walton, K. G., Katta, S., Dalgard, C. L., Sukumar, G., Starr, J., Travis, F. T., Wallace, R. K., Morehead, P., Lonsdorf, N. K., Srivastava, M., & Fagan, J. (2021). Transcriptomics of Long-Term Meditation Practice: Evidence for Prevention or Reversal of Stress Effects Harmful to Health. Medicina (Kaunas, Lithuania), 57(3), 218. https://doi.org/10.3390/medicina57030218
Abstract
Background and Objectives: Stress can overload adaptive mechanisms, leading to epigenetic effects harmful to health. Research on the reversal of these effects is in its infancy. Early results suggest some meditation techniques have health benefits that grow with repeated practice. This study focused on possible transcriptomic effects of 38 years of twice-daily Transcendental Meditation® (TM®) practice. Materials and Methods: First, using Illumina® BeadChip microarray technology, differences in global gene expression in peripheral blood mononuclear cells (PBMCs) were sought between healthy practitioners and tightly matched controls (n = 12, age 65). Second, these microarray results were verified on a subset of genes using quantitative polymerase chain reaction (qPCR) and were validated using qPCR in larger TM and control groups (n = 45, age 63). Bioinformatics investigation employed Ingenuity® Pathway Analysis (IPA®), DAVID, Genomatix, and R packages. Results: The 200 genes and loci found to meet strict criteria for differential expression in the microarray experiment showed contrasting patterns of expression that distinguished the two groups. Differential expression relating to immune function and energy efficiency were most apparent. In the TM group, relative to the control, all 49 genes associated with inflammation were downregulated, while genes associated with antiviral and antibody components of the defense response were upregulated. The largest expression differences were shown by six genes related to erythrocyte function that appeared to reflect a condition of lower energy efficiency in the control group. Results supporting these gene expression differences were obtained with qPCR-measured expression both in the well-matched microarray groups and in the larger, less well-matched groups. Conclusions: These findings are consistent with predictions based on results from earlier randomized trials of meditation and may provide evidence for stress-related molecular mechanisms underlying reductions in anxiety, post-traumatic stress disorder (PTSD), cardiovascular disease (CVD), and other chronic disorders and diseases.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8001870/