Improve the Aging Brain’s Cognition with Mindfulness
By John M. de Castro, Ph.D.
“there is a small but growing body of evidence that regular meditation really can slow ageing – at least at the cellular level.” – James Kingsland
Human life is one of constant change. We revel in our increases in physical and mental capacities during development, but regret their decreases during aging. The aging process involves a systematic progressive decline in every system in the body, the brain included. This includes our mental abilities which decline with age including impairments in memory, attention, problem solving ability, and emotion regulation. It is inevitable and cannot be avoided. There is some hope for these age-related declines, however, as there is evidence that they can be slowed. There are some indications that physical and mental exercise can reduce the rate of cognitive decline and lower the chances of dementia. For example, contemplative practices such as meditation, yoga, and tai chi or qigong have all been shown to be beneficial in slowing or delaying physical and mental decline with aging.
Using modern neuroimaging techniques, scientists have been able to view the changes that occur in the nervous system with aging. In addition, they have been able to investigate various techniques that might slow the process of neurodegeneration that accompanies normal aging. They’ve found that mindfulness practices reduce the deterioration of the brain that occurs with aging restraining the loss of neural tissue. Indeed, the brains of mindfulness practitioners have been found to degenerate less with aging than non-practitioners.
Since the global population of the elderly is increasing at unprecedented rates, it is imperative to investigate methods to slow physical and mental aging and mitigate its effects. In today’s Research News article “Mindful Aging: The Effects of Regular Brief Mindfulness Practice on Electrophysiological Markers of Cognitive and Affective Processing in Older Adults.” See summary below or view the full text of the study at:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5241348/
Malinowski and colleagues recruited individuals between the ages of 55 and 75 years and randomly assigned them to either receive mindfulness training or to an active brain training. Mindfulness training consisted of breath following meditation practice. The brain training condition involved performing mental arithmetic problems that required effortful cognitive processing. Both mindfulness and braining training groups practiced for 10 minutes, 5 days per week, for eight weeks. Before and after training participants were measured for mindfulness, self-efficacy, and mental well-being and were assessed for cognitive and emotion regulation abilities by performance of an eStroop task while their brains’ electrical responses, Electroencephalogram (EEG), were recorded. In the eStroop task the participants viewed a computer screen where one to four words were presented simultaneously. The participants were asked to simply press one of four keys to indicate the number of words presented. There were four conditions; emotionally positive words (love), emotionally negative words (sad), emotionally neutral words (box), and incongruent words. In the incongruent condition the words, one, two, three, or four were presented, with the number of words different from the meaning of the words, e.g. the word three presented two times.
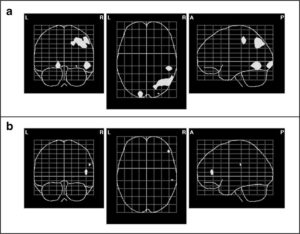
They found that from pre-test to post-test the mindfulness training, but not the brain training group increased in mindfulness and increased their response speed (reaction time) in the eStroop task under all conditions. So, the breath meditation increased mindfulness and made for quicker reactions in the cognitive task. The N2 negative going neural response occurring 0.27 to 0.34 seconds after the presentation of the words, was significantly stronger in the mindfulness than the brain training group. The electrical response was measured over the frontal central cortex, components of the network regulating attention. This result suggests that mindfulness training improves the brains ability to regulate attention.
This study is particularly strong because the control condition was active and required similar commitment of time and energy and belief that the treatment would produce improvements. As a result, the conclusions from the study are very clear. The results suggest that mindfulness training produces improved attentional ability resulting from improved neural responses. These effects were produced in an older group of participants. This suggests that mindfulness training may reduce the cognitive-attentional decline that normally occurs with aging.
This is an exciting proposition, that mindfulness training may improve our ability to cognitively age healthily. As the population continues to live longer and the number of older and elderly individuals increases, the problem of cognitive decline will place an increasing burden on caregivers and stress the healthcare system. So, being able to delay and reduce this decline could have profound effects on individuals and society. Hence, promoting mindfulness training for the elderly could reap substantial benefits for the elderly and the system that supports them in their declining years..
So, improve the aging brain’s cognition with mindfulness.
“Our modern assumptions, ideas, beliefs, and cultural narratives about growing old are too small for us to inhabit. Our thinking about aging is often hijacked by fear, negativity, and ageism. The authentic experience of aging is a source wonder, curiosity, and fascination. Mindful aging is a skillful means to embrace the process of growing older in order to cultivate a deeper understanding and appreciation of the natural flow of all life.” – Brian Alger
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Google+ https://plus.google.com/106784388191201299496/posts and on Twitter @MindfulResearch
Study Summary
Malinowski, P., Moore, A. W., Mead, B. R., & Gruber, T. (2017). Mindful Aging: The Effects of Regular Brief Mindfulness Practice on Electrophysiological Markers of Cognitive and Affective Processing in Older Adults. Mindfulness, 8(1), 78–94. http://doi.org/10.1007/s12671-015-0482-8
Abstract
There is growing interest in the potential benefits of mindfulness meditation practices in terms of counteracting some of the cognitive effects associated with aging. Pursuing this question, the aim of the present study was to investigate the influence of mindfulness training on executive control and emotion regulation in older adults, by means of studying behavioral and electrophysiological changes. Participants, 55 to 75 years of age, were randomly allocated to an 8-week mindful breath awareness training group or an active control group engaging in brain training exercises. Before and after the training period, participants completed an emotional-counting Stroop task, designed to measure attentional control and emotion regulation processes. Concurrently, their brain activity was measured by means of 64-channel electroencephalography. The results show that engaging in just over 10 min of mindfulness practice five times per week resulted in significant improvements in behavioral (response latency) and electrophysiological (N2 event-related potential) measures related to general task performance. Analyses of the underlying cortical sources (Variable Resolution Electromagnetic Tomography, VARETA) indicate that this N2-related effect is primarily associated with changes in the right angular gyrus and other areas of the dorsal attention network. However, the study did not find the expected specific improvements in executive control and emotion regulation, which may be due to the training instructions or the relative brevity of the intervention. Overall, the results indicate that engaging in mindfulness meditation training improves the maintenance of goal-directed visuospatial attention and may be a useful strategy for counteracting cognitive decline associated with aging.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5241348/