Improve Post-Traumatic Stress Disorder (PTSD) Symptoms with Loving Kindness Meditation
By John M. de Castro, Ph.D.
“You probably know that symptoms of posttraumatic stress disorder (PTSD) often include anxiety, unwanted memories, anger and avoidance. But did you know that meditation may be able to help? Meditative practices have been linked to decreases in hyperarousal, depression and insomnia.” – Jill Bormann
Experiencing trauma is quite common. It has been estimated that 60% of men and 50% of women will experience a significant traumatic event during their lifetime. But only a fraction will develop Post-Traumatic Stress Disorder (PTSD). But this still results in a frightening number of people with 7%-8% of the population developing PTSD at some point in their life. For military personnel, it’s much more likely for PTSD to develop with about 11%-20% of those who have served in a war zone developing PTSD.
PTSD involves a number of troubling symptoms including reliving the event with the same fear and horror in nightmares or with a flashback. PTSD sufferers avoid situations that remind them of the event this may include crowds, driving, movies, etc. and may avoid seeking help because it keeps them from having to think or talk about the event. They often experience negative changes in beliefs and feelings including difficulty experiencing positive or loving feelings toward other people, avoiding relationships, memory difficulties, or see the world as dangerous and no one can be trusted. Sufferers may feel hyperarousal, feeling keyed up and jittery, or always alert and on the lookout for danger. They may experience sudden anger or irritability, may have a hard time sleeping or concentrating, may be startled by a loud noise or surprise.
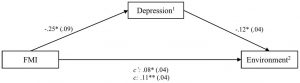
Obviously, these are troubling symptoms that need to be addressed. There are a number of therapies that have been developed to treat PTSD. One of which, mindfulness training has been found to be particularly effective. Increasing self-compassion is important for improvement in PTSD symptoms. Mindfulness has been shown to increase self-compassion. In Loving Kindness Meditation the individual systematically pictures different individuals from self, to close friends, to enemies and wishes them happiness, well-being, safety, peace, and ease of well-being. So, Loving Kindness Meditation may be an effective treatment for the symptoms of PTSD.
In today’s Research News article “Loving-Kindness Meditation vs Cognitive Processing Therapy for Posttraumatic Stress Disorder Among Veterans: A Randomized Clinical Trial.” (See summary below or view the full text of the study at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8052593/ ) Kearney and colleagues recruited military veterans who were diagnosed with Post-Traumatic Stress Disorder (PTSD) and randomly assigned them to receive 2 weekly 90-minute group sessions of either Loving Kindness Meditation or Cognitive Processing Therapy (CPT). CPT “combines cognitive restructuring with emotional processing of trauma-related content”. They were measured before and after treatment and 3 and 6 months later for PTSD symptom severity and depression.
They found that in comparison to baseline both groups had significant but modest reductions in PTSD symptom severity and depression that were maintained 6 months after the end of treatment. The therapy groups did not differ in PTSD symptom severity but the group that practiced Loving Kindness Meditation had significantly lower level of depression after treatment and 6 months later.
These are interesting findings that suggest that both Loving Kindness Meditation and Cognitive Processing Therapy (CPT) produce modest relief of the symptoms of PTSD and depression in military veterans. But Loving Kindness Meditation produces better outcomes in relieving depression. Loving Kindness Meditation is known to improve mindfulness and compassion for the self and others, and this appears to help relieve the psychological consequences of trauma. This suggests that trauma, to some extent, produces a degree of self-blame which may be responsible for some of the symptoms. But these therapies produce only modest improvements suggesting that Loving Kindness Meditation is not a cure but may be useful as a component in the treatment of PTSD.
So, improve Post-Traumatic Stress Disorder (PTSD) symptoms with Loving Kindness Meditation.
“veteran participants self-reported a significant decrease in their PTSD symptoms and a high degree of satisfaction with the compassion meditation program.” – Laura McArdle
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Google+ https://plus.google.com/106784388191201299496/posts and on Twitter @MindfulResearch
Study Summary
Kearney, D. J., Malte, C. A., Storms, M., & Simpson, T. L. (2021). Loving-Kindness Meditation vs Cognitive Processing Therapy for Posttraumatic Stress Disorder Among Veterans: A Randomized Clinical Trial. JAMA network open, 4(4), e216604. https://doi.org/10.1001/jamanetworkopen.2021.6604
Question
Is group loving-kindness meditation noninferior to group cognitive processing therapy for treatment of posttraumatic stress disorder (PTSD) among veterans?
Findings
In this randomized clinical trial, 184 veterans with PTSD were assigned to group loving-kindness meditation or group cognitive processing therapy; the differences in the decrease from baseline to 6-month follow-up for measures of PTSD and depression were very similar and within predefined margins considered not meaningfully different. Attendance was better for loving-kindness meditation.
Meaning
This study adds to the evidence indicating that interventions without a specific focus on trauma, including meditation-based interventions, can yield results similar to trauma-focused therapies.
Importance
Additional options are needed for treatment of posttraumatic stress disorder (PTSD) among veterans.
Objective
To determine whether group loving-kindness meditation is noninferior to group cognitive processing therapy for treatment of PTSD.
Design, Setting, and Participants
This randomized clinical noninferiority trial assessed PTSD and depression at baseline, posttreatment, and 3- and 6-month follow-up. Veterans were recruited from September 24, 2014, to February 5, 2018, from a large Veternas Affairs medical center in Seattle, Washington. A total of 184 veteran volunteers who met Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition) criteria for PTSD were randomized. Data collection was completed November 28, 2018, and data analyses were conducted from December 10, 2018, to November 5, 2019.
Interventions
Each intervention comprised 12 weekly 90-minute group sessions. Loving-kindness meditation (n = 91) involves silent repetition of phrases intended to elicit feelings of kindness for oneself and others. Cognitive processing therapy (n = 93) combines cognitive restructuring with emotional processing of trauma-related content.
Main Outcomes and Measures
Co–primary outcomes were change in PTSD and depression scores over 6-month follow-up, assessed by the Clinician-Administered PTSD Scale (CAPS-5; range, 0-80; higher is worse) and Patient-Reported Outcome Measurement Information System (PROMIS; reported as standardized T-score with mean [SD] of 50 [10] points; higher is worse) depression measures. Noninferiority margins were 5 points on the CAPS-5 and 4 points on the PROMIS depression measure.
Results
Among the 184 veterans (mean [SD] age, 57.1 [13.1] years; 153 men [83.2%]; 107 White participants [58.2%]) included in the study, 91 (49.5%) were randomized to the loving-kindness group, and 93 (50.5%) were randomized to the cognitive processing group. The mean (SD) baseline CAPS-5 score was 35.5 (11.8) and mean (SD) PROMIS depression score was 60.9 (7.9). A total of 121 veterans (66%) completed 6-month follow-up. At 6 months posttreatment, mean CAPS-5 scores were 28.02 (95% CI, 24.72-31.32) for cognitive processing therapy and 25.92 (95% CI, 22.62-29.23) for loving-kindness meditation (difference, 2.09; 95% CI, −2.59 to 6.78), and mean PROMIS depression scores were 61.22 (95% CI, 59.21-63.23) for cognitive processing therapy and 58.88 (95% CI, 56.86-60.91) for loving-kindness meditation (difference, 2.34; 95% CI, −0.52 to 5.19). In superiority analyses, there were no significant between-group differences in CAPS-5 scores, whereas for PROMIS depression scores, greater reductions were found for loving-kindness meditation vs cognitive processing therapy (for patients attending ≥6 visits, ≥4-point improvement was noted in 24 [39.3%] veterans receiving loving-kindness meditation vs 9 (18.0%) receiving cognitive processing therapy; P = .03).
Conclusions and Relevance
Among veterans with PTSD, loving-kindness meditation resulted in reductions in PTSD symptoms that were noninferior to group cognitive processing therapy. For both interventions, the magnitude of improvement in PTSD symptoms was modest. Change over time in depressive symptoms was greater for loving-kindness meditation than for cognitive processing therapy.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8052593/