Mindfulness is Associated with Improved Symptoms of Schizophrenia
By John M. de Castro, Ph.D.
“schizophrenia patients may benefit from mindfulness-based interventions because they . . . demonstrate strong relationships between mindfulness and psychological constructs related to adaptive functioning.” – Naomi T. Tabak
Schizophrenia is the most common form of psychosis. Its effects about 1% of the population worldwide. It appears to be highly heritable and involves changes in the brain. It is characterized by both positive and negative symptoms. Positive symptoms include hallucinations; seeing and, in some cases, feeling, smelling or tasting things that aren’t there, or delusions; unshakable beliefs that, when examined rationally, are obviously untrue. Negative symptoms include a reduced ability to function normally, neglect of personal hygiene, lack of emotion, blank facial expressions, speaking in a monotone, loss of interest in everyday activities, social withdrawal, an inability to experience pleasure, and a lack of insight into their symptoms. The symptoms of schizophrenia usually do not appear until late adolescence or early adulthood.
Schizophrenia is very difficult to treat with psychotherapy and is usually treated with antipsychotic drugs. These drugs, however, are not always effective, sometimes lose effectiveness, and can have some difficult side effects. Mindfulness training has been shown to be beneficial for a variety of mental health problems, including psychosis. Mindfulness has also been shown to associated with lower symptom severity of schizophrenia. So, it makes sense to study the relationships of mindfulness with the symptoms of schizophrenia.
In today’s Research News article “The Relationship Between Mindfulness, Depression, Anxiety, and Quality of Life in Individuals With Schizophrenia Spectrum Disorders.” (See summary below or view the full text of the study at: https://www.frontiersin.org/articles/10.3389/fpsyg.2021.708808/full?utm_source=F-AAE&utm_medium=EMLF&utm_campaign=MRK_1721400_a0P58000000G0YfEAK_Psycho_20210909_arts_A ) Bergmann and colleagues recruited patients who were diagnosed with schizophrenia and measured them for mindfulness, anxiety, depression, perceived stress, and quality of life.
They found that the higher the levels of mindfulness, the lower the levels of anxiety, depression, and perceived stress and the higher the levels of quality of life. In addition, they found that the higher the levels of anxiety, depression, and perceived stress the lower the levels of quality of life. A mediation analysis found that mindfulness was positively related to quality of life directly and also indirectly by being associated with lower levels of anxiety and depression that were in turn associated with higher quality of life.
This study is correlational and as such causation cannot be determined. But, previous controlled research has demonstrated the mindfulness training produces lower levels of anxiety and depression and higher levels of quality of life. So the present results are likely due to causal effects of mindfulness. Hence, being mindful improves quality of life and decreases anxiety and depression which then also improve quality of life. These are similar findings to those seen in healthy individuals. So, the present findings suggest that mindfulness affects people with schizophrenia in a similar fashion. They further suggest that mindfulness training might improve the psychological health and well-being of patients with schizophrenia.
So, mindfulness is associated with improved symptoms of schizophrenia.
“mindfulness-based interventions for psychotic symptoms can afford people a greater acceptance and insight into their experiences. They can also reduce the symptoms of anxiety and depression which often accompany, and may exacerbate, psychotic disorders.” – Adrianna Mendrek
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Google+ https://plus.google.com/106784388191201299496/posts and on Twitter @MindfulResearch
Study Summary
Bergmann N, Hahn E, Hahne I, Zierhut M, Ta TMT, Bajbouj M, Pijnenborg GHM and Böge K (2021) The Relationship Between Mindfulness, Depression, Anxiety, and Quality of Life in Individuals With Schizophrenia Spectrum Disorders. Front. Psychol. 12:708808. doi: 10.3389/fpsyg.2021.708808
Background: Schizophrenia spectrum disorders (SSD) are frequently accompanied by comorbid depressive and anxiety symptoms, as well as impaired quality of life (QoL). A growing body of evidence has demonstrated the relevance of mindfulness for SSD in recent years. The study examined the association between mindfulness, depression, anxiety, and QoL.
Materials and Methods: A total of 83 participants with SSD were recruited at the in- and outpatient psychiatric hospital care. Participants completed the Southampton Mindfulness Questionnaire, Comprehensive Inventory for Mindful Experiences, and Freiburger Mindfulness Inventory, the Depression, Anxiety, Stress Scale to assess depression and anxiety, and the WHO-QoL Questionnaire. Multiple regression analyses examined the relationship between mindfulness and QoL and the mediating role of depression and anxiety.
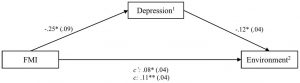
Results: Mindfulness had a significant statistical positive effect on QoL domains physical health, psychological, and environmental QoL in patients with SSD. Depression was identified as a significant mediator of this relationship.
Conclusion: This study provides novel insight into mindfulness’ mechanisms and paves the way for a process-oriented approach to treat SSD. The results provide first evidence for the process-based value of mindfulness for SSD; future studies can focus on the role of mindfulness for central therapeutic processes of change by employing longitudinal designs.