Reduce Inflammation in Mildly Cognitive Impaired Elderly with Mindfulness
By John M. de Castro, Ph.D.
“Mindfulness practice was not directly linked to lower inflammation levels, but may have bolstered stress resilience among at-risk adults by preventing an increase in inflammatory biomarker levels.” – Grace Bullock
The immune system is designed to protect the body from threats like stress, infection, injury, and toxic chemicals. One of its tools is the Inflammatory response. This response works quite well for short-term infections and injuries. But when inflammation is protracted and becomes chronic, it can itself become a threat to health. It can produce autoimmune diseases such as colitis, Chron’s disease, arthritis, heart disease, increased cancer risk, lung disease, sleep disruption, gum disease, decreased bone health, psoriasis, and depression. In the elderly it is associated with the onset of dementia.
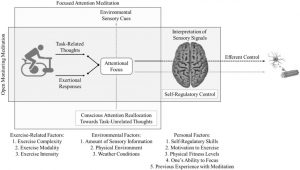
Needless to say, chronic inflammation can create major health problems. Indeed, the presence of chronic inflammation is associated with reduced longevity. So, it is important for health to control the inflammatory response, allowing it to do its job in fighting off infection but reducing its activity when no external threat is apparent. Of course, it is far better to prevent chronic inflammation in the first place than to treat it later. Mind-body techniques such as yoga, Tai Chi and meditation have been shown to adaptively reduce the inflammatory response. Mindfulness training, then, may reduce the prospect of the development of dementia by reducing the inflammatory response.
In today’s Research News article “Mindfulness improves inflammatory biomarker levels in older adults with mild cognitive impairment: a randomized controlled trial.” (See summary below or view the full text of the study at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7026149/), Ng and colleagues recruited elderly (> 60 years of age) who had mild cognitive impairment but not dementia and randomly assigned them to receive once a week for 1 hour for 12 weeks of either health education or mindfulness awareness practice. For the next 6 months they received monthly booster sessions. The mindfulness awareness practice was based upon the Mindfulness-Based Stress Reduction (MBSR) program adapted for the elderly. The participants were also instructed to practice daily at home. Before and after training and 6 months later the participants contributed blood samples that were assayed for inflammatory biomarkers of high-sensitivity (hs)-CRP, BDNF, and DHEA-S. They also contributed salivary samples that were assayed for the inflammatory biomarkers of cortisol, IL-1β, and IL-6.
They found that in comparison to baseline and the health education group, the elderly participants who received mindfulness training had significantly lower blood levels of high-sensitivity (hs)-CRP at the end of training and 6 months later. This effect was particularly strong in female participants. Male participants had significantly reduced IL-6 and IL-1β levels at the end of training.
These findings are potentially very important. high-sensitivity (hs)-CRP has been associated with the onset of dementia. Hence, mindfulness training may significantly reduce this risk factor for dementia. Mindfulness training has been shown to improve the symptoms of dementia. The present findings suggest that mindfulness training may work to improve dementia by lowering high-sensitivity (hs)-CRP. It remains for future research to investigate this tantalizing prospect.
The results suggest that mindfulness training reduce biomarkers of inflammation in the elderly with mild cognitive impairment. Inflammation is characteristic of dementia. The results suggest that mindfulness training may reduce the likelihood that mild cognitive impairment develops into full-fledged dementia by reducing inflammation in the elderly. Regardless, the reduction in inflammation would be predicted to improve the overall health and longevity of the elderly.
So, reduce inflammation in mildly cognitive impaired elderly with mindfulness.
“Meditation is associated with many psychological and physical benefits. “In general, it’s been shown to decrease blood pressure and inflammation.” – Heidi Goldman
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Google+ https://plus.google.com/106784388191201299496/posts and on Twitter @MindfulResearch
Study Summary
Ng, T., Fam, J., Feng, L., Cheah, I. K., Tan, C. T., Nur, F., Wee, S. T., Goh, L. G., Chow, W. L., Ho, R. C., Kua, E. H., Larbi, A., & Mahendran, R. (2020). Mindfulness improves inflammatory biomarker levels in older adults with mild cognitive impairment: a randomized controlled trial. Translational psychiatry, 10(1), 21. https://doi.org/10.1038/s41398-020-0696-y
Abstract
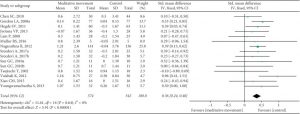
Few randomized controlled trials investigated the effects of mindfulness intervention on older adults diagnosed with mild cognitive impairment (MCI). Furthermore, there have been hypotheses and theoretical mechanisms on the benefits of mindfulness intervention on biomarkers of stress, inflammation, and neuroplasticity implicated in MCI that warrant empirical evidence. We conducted a pilot randomized controlled trial to examine whether Mindful Awareness Practice (MAP) improved biomarker levels in older adults with MCI. Fifty-five community-dwelling older adults aged 60 and above were randomized into either the treatment arm, MAP, or the active control arm, the health education program (HEP). Researchers who were blinded to treatment allocation assessed the outcomes at baseline, 3-month, and 9-month follow-ups. Linear-mixed models were used to examine the effect of MAP on biomarker levels. MAP participants had significantly decreased high-sensitivity c-reactive protein (hs-CRP) levels at 9-month (β = −0.307, 95% CI = −0.559 to −0.054 P = 0.018). Exploratory sub-group analyses by sex showed significantly decreased hs-CRP in females only (β = −0.445, 95% CI = −0.700 to −0.189, P = 0.001), while stratification by MCI subtype showed hs-CRP decreased only in amnestic-MCI (aMCI) (β = −0.569, 95% CI = −1.000 to −0.133, P = 0.012). Although total sample analyses were not significant, males had significantly decreased interleukin (IL)−6 (β = −1.001, 95% CI = −1.761 to −0253, P = 0.011) and IL-1β (β = −0.607, 95% CI = −1.116 to −0.100, P = 0.021) levels at 3-month and non-significant improvements at 9-month time-point. MAP improved inflammatory biomarkers in sex- and MCI subtype-specific manners. These preliminary findings suggest the potential of mindfulness intervention as a self-directed and low-cost preventive intervention in improving pathophysiology implicated in MCI.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7026149/