Improve Cognition and Performance in 3rd Grade Children with Mindfulness
By John M. de Castro, Ph.D.
“The Collaborative for Academic, Social, and Emotional Learning (CASEL) has linked mindfulness to two core social-emotional skills: self-regulation and self-awareness. Skills in these areas teach students not only how to recognize their thoughts, emotions, and actions, but also how to react to them in positive ways.” – Waterford.org
Childhood is a miraculous period during which the child is dynamically absorbing information from every aspect of its environment. This is particularly evident during the elementary school years. Mindfulness training in school has been shown to have very positive effects. These include improvements in the academic, cognitive, psychological, and social domains. Training early in childhood has the potential of jump-starting the child’s academic performance.
In today’s Research News article “Promoting Third Graders’ Executive Functions and Literacy: A Pilot Study Examining the Benefits of Mindfulness vs. Relaxation Training.” (See summary below or view the full text of the study at: https://www.frontiersin.org/articles/10.3389/fpsyg.2021.643794/full?utm_source=F-AAE&utm_medium=EMLF&utm_campaign=MRK_1645362_69_Psycho_20210525_arts_A ) Cordeiro and colleagues recruited 3rd grade students and randomly assigned them to receive 2 30-minute sessions per week for 8 weeks of either mindfulness training or progressive muscle relaxation training. They were measured before and after training for non-verbal intelligence, short-term memory, inhibitory control, and cognitive flexibility, teacher ratings of the child’s short-term memory, inhibitory control, and cognitive flexibility, handwriting fluency, spelling, essay quality, and school grades.
They found that for children low in executive function, relaxation training produced significantly greater improvement in executive function while students high in executive function, mindfulness training produced significantly greater improvement in executive function. Further, in children high in cognitive flexibility mindfulness training produced significantly greater improvement in cognitive flexibility. Finally, they found that mindfulness training produced significantly greater improvements in handwriting fluency and school grades than relaxation training.
The results were not as straightforward as one might like but still are interesting. They suggest that mindfulness training of 3rd grade students produces cognitive improvements in the students with the greatest cognitive ability to start with and significantly greater improvements in grades and handwriting fluency in all students. It should be noted that there was no follow-up beyond the end of training, so it is not known if the benefits of mindfulness training persist longer than immediately after training.
It has been demonstrated in previous research that mindfulness training produces improvement in cognition and school performance. The results of the present study suggest that mindfulness training is beneficial for young children in the 3rd grade improving their thinking ability and school performance. Early interventions in children’s lives and school performance have the potential of producing greater achievements as the child progresses through school. It remains for future research to determine the long-term effects of early mindfulness training.
So, improve cognition and performance in 3rd grade children with mindfulness.
“Mindfulness applies to nearly every part of life. It includes everything from mindful commuting, to being mindful of what we eat (and how it smells and tastes) to being mindful of opportunities to sneak in some physical activity – or rest – during our busy days. And for adults, a good place to start learning the art of mindfulness is from these third graders!” – Health Partners
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Google+ https://plus.google.com/106784388191201299496/posts and on Twitter @MindfulResearch
Study Summary
Cordeiro C, Magalhães S, Rocha R, Mesquita A, Olive T, Castro SL and Limpo T (2021) Promoting Third Graders’ Executive Functions and Literacy: A Pilot Study Examining the Benefits of Mindfulness vs. Relaxation Training. Front. Psychol. 12:643794. doi: 10.3389/fpsyg.2021.643794
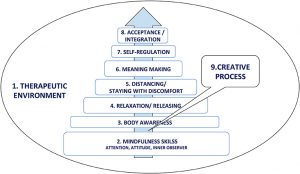
Research suggested that developing mindfulness skills in children improves proximal outcomes, such as attention and executive functions, as well as distal outcomes, such as academic achievement. Despite empirical evidence supporting this claim, research on the benefits of mindfulness training in child populations is scarce, with some mixed findings in the field. Here, we aimed to fill in this gap, by examining the effects of a mindfulness training on third graders’ proximal and distal outcomes, namely, attention and executive functions (viz., inhibitory control, working memory, and cognitive flexibility) as well as literacy-related achievement (viz., handwriting fluency, text quality, Portuguese grades). These outcomes were measured with behavioral tasks and teacher ratings. Sixty-six Portuguese children were randomly allocated to an experimental group receiving mindfulness training (n = 29) or an active control group receiving relaxation training (n = 37). Both training programs were implemented by psychologists in two 30-min weekly sessions for 8 weeks. All students were assessed before and after the interventions. Three main findings are noteworthy: (a) mindfulness training enhanced teacher-rated cognitive flexibility and a performance-based composite score of executive functions among children with higher pretest scores; (b) relaxation training improved performance-based cognitive flexibility and the composite score of executive functions among children with lower pretest scores; (c) children receiving mindfulness training had higher handwriting fluency and better grades in Portuguese than those receiving relaxation training. These findings provide preliminary evidence on the benefits of mindfulness training in educational settings and highlight the moderating role of baseline performance on those benefits.