Increase Quality of Life and Decrease Weight of Patients with Diabetes with Tai Chi
By John M. de Castro, Ph.D.
“a regular tai chi exercise program may help lower blood glucose levels, allowing people with diabetes to better control their disease.” – Lindsey Getz
Diabetes is a major health issue. It is estimated that 30 million people in the United States have diabetes and the numbers are growing. Type 2 Diabetes results from a resistance of tissues, especially fat tissues, to the ability of insulin to promote the uptake of glucose from the blood. As a result, blood sugar levels rise producing hyperglycemia. Diabetes is the 7th leading cause of death in the United States. In addition, diabetes is heavily associated with other diseases such as cardiovascular disease, heart attacks, stroke, blindness, kidney disease, and circulatory problems leading to amputations. As a result, diabetes doubles the risk of death of any cause compared to individuals of the same age without diabetes.
Type 2 diabetes is largely preventable. One of the reasons for the increasing incidence of Type 2 Diabetes is its association with overweight and obesity which is becoming epidemic in the industrialized world. A leading cause of this is a sedentary life style. Current treatments for Type 2 Diabetes focus on diet, exercise, and weight control. Recently, mindfulness practices have been shown to be helpful in managing diabetes. Tai Chi is mindfulness practice and a gentle exercise that has been found to improve the symptoms of Type 2 Diabetes. The research is accumulating. So, it is reasonable to examine what has been learned.
In today’s Research News article “Effect of Tai Chi on Quality of Life, Body Mass Index, and Waist-Hip Ratio in Patients With Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis.” (See summary below or view the full text of the study at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7851054/ ) Qin and colleagues review, summarize, and perform a meta-analysis of the published research studies of the effectiveness of Tai Chi practice in the treatment of Type 2 Diabetes. They found 18 published research studies, 15 of which were randomized controlled studies.
They report that the published research found that patients with Type 2 Diabetes who practiced Tai Chi had significant improvements in their quality of life including physical function, pain, overall health, vitality, social function, emotional function, and mental health dimensions. The research also found that Tai Chi practice produced significant reductions in body size as reflected in the waist-hip ration and the body mass index (BMI), but the improvements were equivalent to that produced by other aerobic exercises.
These are important findings as Type 2 Diabetes is so impactful on the health and longevity of large numbers of patients. The results suggest that Tai Chi practice reduces body size which is very important in improving metabolic and glucose control. As a consequence, it greatly improves the quality of life of the patients. It appears from the research that the exercise component of Tai Chi practice is important for the improvements as other aerobic exercises produce similar effects.
Some advantages of Tai Chi practice include the facts that it is not strenuous, involves slow gentle movements, and is safe, having no appreciable side effects, it is appropriate for all ages including the elderly and for individuals with illnesses that limit their activities or range of motion. It can also be practiced without professional supervision and in groups making it inexpensive to deliver and fun to engage in. This makes Tai Chi practice an excellent means to improve the physical and psychological symptoms experienced by patients with Type 2 Diabetes.
So, increase quality of life and decrease weight of patients with diabetes with Tai Chi.
“Tai Chi exercises can improve blood glucose levels and improve the control of type 2 diabetes and immune system response.” – Anna Sophia McKenney
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Google+ https://plus.google.com/106784388191201299496/posts and on Twitter @MindfulResearch
Study Summary
Qin, J., Chen, Y., Guo, S., You, Y., Xu, Y., Wu, J., Liu, Z., Huang, J., Chen, L., & Tao, J. (2021). Effect of Tai Chi on Quality of Life, Body Mass Index, and Waist-Hip Ratio in Patients With Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis. Frontiers in endocrinology, 11, 543627. https://doi.org/10.3389/fendo.2020.543627
Abstract
Background
Type 2 diabetes mellitus (T2DM) is a worldwide public health concern with high morbidity and various progressive diabetes complications that result in serious economic expenditure and social burden. This systematic review aims to evaluate the effect of Tai Chi on improving quality of life (QoL), body mass index (BMI) and waist-hip ratio (WHR) in patients with T2DM.
Method
A systematic review and meta-analysis was performed following PRISMA recommendation. Four English databases and three Chinese databases were searched. The PEDro scale was used to assess the methodological quality of including studies. Study inclusion criteria: randomized controlled trials (RCTs) and quasi-experimental studies were included, patients with T2DM that adopted Tai Chi as intervention and QoL, BMI and/or WHR as outcome measurements.
Results
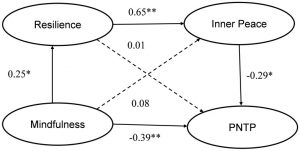
Eighteen trials were included. The aggregated results of seven trials showed that Tai Chi statistically significantly improved QoL measured by the SF-36 on every domains (physical function: MD = 7.73, 95% confidence interval (CI) = 1.76 to 13.71, p = 0.01; role-physical function: MD = 9.76, 95% CI = 6.05 to 13.47, p < 0.001; body pain: MD = 8.49, 95% CI = 1.18 to 15.8, p = 0.02; general health: MD = 9.80, 95% CI = 5.77 to 13.82, p < 0.001; vitality: MD = 6.70, 95% CI = 0.45 to 12.94, p = 0.04; social function: MD = 9.1, 95% CI = 4.75 to 13.45, p < 0.001; role-emotional function: MD = 7.88, 95% CI = 4.03 to 11.72, p < 0.001; mental health: MD = 5.62, 95% CI = 1.57 to 9.67, p = 0.006) and BMI (MD = −1.53, 95% CI = −2.71 to −0.36, p < 0.001) compared with control group (wait list; no intervention; usual care; sham exercise).
Conclusion
Tai Chi could improve QoL and decrease BMI for patients with T2DM, more studies are needed to be conducted in accordance with suggestions mentioned in this review.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7851054/