Improve Mental Health with Mindfulness
By John M. de Castro, Ph.D.
“If you want to conquer the anxiety of life, live in the moment, live in the breath.”
― Amit Ray
Over the last several decades, research and anecdotal experiences have accumulated an impressive evidential case that the development of mindfulness has positive benefits for the individual’s mental, physical, and spiritual life. Mindfulness appears to be beneficial both for healthy people and for people suffering from a myriad of mental and physical illnesses. It appears to be beneficial across ages, from children to the elderly. And it appears to be beneficial across genders, personalities, race, and ethnicity. The breadth and depth of benefits is unprecedented. There is no other treatment or practice that has been shown to come anyway near the range of mindfulness’ positive benefits.
Over the last few decades, a vast amount of research has been published on the benefits of mindfulness practices on the mental and physical health of the practitioners. Most of these studies, however, utilize momentary (one-time) measures of mindfulness. A better method may be to measure mindfulness over a sustained period of time. Many studies have been performed using mindfulness measurement over time. So, it makes sense to step back and summarize what has been learned.
In today’s Research News article “Associations between mindfulness and mental health outcomes: A systematic review of ecological momentary assessment research.” (See summary below or view the full text of the study at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9187214/ ) Enkema and colleagues
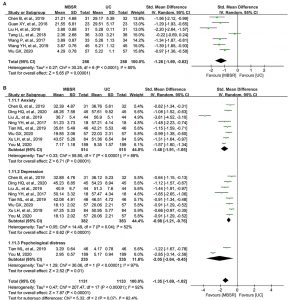
Review and summarize the published research studies on the benefits of mindfulness measured over time on mental health. They identified 22 published research studies.
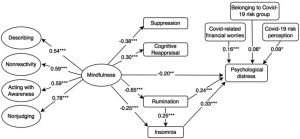
They report that the published research found that mindfulness, measured over a sustained period of time, was associated with improved mental health. This included improvements in emotional awareness and positive emotions and decreases in negative emotions, anxiety, depression, rumination, cravings, and self-harm. Some indications were reported that measurement over sustained periods of time have greater reliability and validity.
“The way to live in the present is to remember that ‘This too shall pass.’ When you experience joy, remembering that ‘This too shall pass’ helps you savor the here and now. When you experience pain and sorrow, remembering that ‘This too shall pass’ reminds you that grief, like joy, is only temporary.” – Joey Green
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Twitter @MindfulResearch
Study Summary
Enkema MC, McClain L, Bird ER, Halvorson MA, Larimer ME. Associations between mindfulness and mental health outcomes: A systematic review of ecological momentary assessment research. Mindfulness (N Y). 2020 Nov;11(11):2455-2469. doi: 10.1007/s12671-020-01442-2. Epub 2020 Jul 15. PMID: 35694042; PMCID: PMC9187214.
Abstract
Objectives:
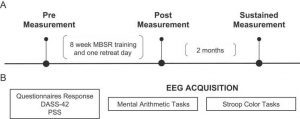
Psychological science has taken up investigations of the effectiveness of mindfulness-based programs (MBPs) and mechanisms through which people benefit from mindfulness. Reliable and valid psychometric tools are essential components of psychological science, and efforts have been made to produce tools for the accurate measurement of mindfulness as a construct. However, trait measurement methods, which are commonly used, may not adequately assess mindfulness and mental health outcomes in a way that allows for mechanisms to be adequately tested. Intensive longitudinal assessment methods sample behavior and experience multiple times over a brief period of several days or weeks, and may be more appropriate methods for testing mechanisms of action. We provide a systematic review of published, peer-reviewed studies that used intensive longitudinal methods to investigate the effects of mindfulness on mental health outcomes.
Methods:
Articles were included in the systematic review if mindfulness measures and/or mindfulness interventions were a part of the study design and if intensive longitudinal methods were used to assess mindfulness or mental health outcomes.
Results:
Findings consistently demonstrated a positive association between mindfulness and mental health. Only two studies collected both trait and state measurements of either mindfulness or mental health outcomes, and results indicated that EMA produced larger effect sizes between mindfulness and mental health outcomes.
Conclusions:
Theorized associations between mindfulness and mental health are supported by the current EMA literature. Intensive longitudinal methods may produce more consistent and reliable results through increased sensitivity and ecological validity in that they examine the momentary relationships between mindfulness and mental health outcomes. Thus, intensive longitudinal assessment may be a more appropriate method for investigating hypothesized mechanisms of action in MBPs.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9187214/