By John M. de Castro, Ph.D.
“But for many patients dealing with depression, anxiety, or stress, yoga may be a very appealing way to better manage symptoms. Indeed, the scientific study of yoga demonstrates that mental and physical health are not just closely allied, but are essentially equivalent. The evidence is growing that yoga practice is a relatively low-risk, high-yield approach to improving overall health.” – Harvard Mental Health Letter
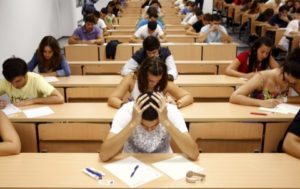
Many people have fond memories of their college years. It is likely, however, that they forgot about the stress and angst of those years. The truth is that college is generally very stressful for most students, from the uncertainty of freshman year, to the social stresses of emerging adulthood, to the anxiety of launching into a career after senior year. Evidence for the difficulties of these years can be found in college counseling centers which are swamped with troubled students. In fact, it’s been estimated that half of all college students report significant levels of anxiety and depression.
In recent years, it has become apparent that contemplative practices are powerful treatment options for depression and anxiety disorders either alone or in combination with other therapies. Both mindfulness training and yoga practice have been found to be effective. But, there has not been a direct comparison. In today’s Research News article “Controlled Trial of Mindfulness Versus Yoga: Effects on Depression and/or Anxiety in College Students.” See:
or see summary below, Falsafi recruited college students, with a diagnosis of wither anxiety disorder or depression, and randomly assigned them to receive 8 weeks, 75 minutes per week, plus 20 minutes per day of home practice, of either mindfulness training or Hatha yoga practice, or to a no-treatment control condition. All groups also continued their usual treatments of drugs or psychotherapy. The students were assessed for mindfulness, depression, anxiety, stress, and self-compassion prior to treatment, mid treatment (week 4), the end of treatment (week 8) and a follow-up at week 12.
They found that in comparison to the no-treatment control condition both the mindfulness training and yoga practice groups had significant decreases in anxiety, depression, and stress, and increases in mindfulness and these improvements were maintained at the 12-week follow-up. There were no significant differences found between the effects of mindfulness training or yoga practice, except that only the mindfulness training groups showed a significant increase in self-compassion. This latter difference was probably due to the fact that the mindfulness training included specific exercises to improve self-compassion including loving-kindness meditation practice.
These findings confirm previous findings that both mindfulness training and yoga practice produce clinically significant improvements in mindfulness, anxiety, depression, and stress, and that mindfulness improves self-compassion. The interesting aspect of this study is that comparable amounts of mindfulness and yoga practice did not differ in effectiveness. This is useful as different people prefer mindfulness training or yoga practice. So, individuals with anxiety and depression can choose which practice they are most comfortable with. This should increase participation and compliance and as a result effectiveness.
So, reduce anxiety and depression with mindfulness and yoga.
“People with anxiety have a problem dealing with distracting thoughts that have too much power. They can’t distinguish between a problem-solving thought and a nagging worry that has no benefit. If you have unproductive worries, you can train yourself to experience those thoughts completely differently. You might think ‘I’m late, I might lose my job if I don’t get there on time, and it will be a disaster!’ Mindfulness teaches you to recognize, ‘Oh, there’s that thought again. I’ve been here before. But it’s just that—a thought, and not a part of my core self,’” – Elizabeth Hoge
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Google+ https://plus.google.com/106784388191201299496/posts
Study Summary
Falsafi N. A Randomized Controlled Trial of Mindfulness Versus Yoga: Effects on Depression and/or Anxiety in College Students. J Am Psychiatr Nurses Assoc. 2016 Aug 26. pii: 1078390316663307. [Epub ahead of print]
Abstract
BACKGROUND: Depression and anxiety disorders are two of the most common mental disorders in the United States. These disorders are prevalent among college students.
OBJECTIVE: The main objective of this study is to compare the effectiveness of two different types of intervention practices (mindfulness vs. yoga) and a noninterventional control group in mitigating the effects of depression and/or anxiety in college students.
METHOD: A sample of 90 students (both genders) over age 18 who had a diagnosis of anxiety and/or depression was recruited from 11,500 undergraduate college students in a mid-size university. The study’s design included stratified-randomized controlled repeated measures with three groups: a mindfulness intervention group, a yoga-only intervention group, and a noninterventional group. Participants were randomly assigned to the aforementioned three groups. Participants in the intervention groups received an 8-week training either in mindfulness or yoga. Depressive, anxiety, stress symptoms, self-compassion, and mindfulness were measured at baseline, Week 4, Week 8, and Week 12.
RESULTS: Depressive, anxiety, and stress symptoms decreased significantly (p < .01) from baseline to follow-up conditions in both the mindfulness and yoga intervention groups. The changes in mindfulness scores were also significant in both groups. However, the changes in self-compassion scores were significant only in the mindfulness intervention group. No significant changes in the control group were demonstrated.
CONCLUSIONS: The findings from this study can provide useful information to nurses and other health care providers. This study may have implications for a cost-effective treatment for depression and anxiety.