Meditation Strengthens Brain Attentional Networks
By John M. de Castro, Ph.D.
“meditation practice appears to positively impact attentional functions by improving resource allocation processes. As a result, attentional resources are allocated more fully during early processing phases which subsequently enhance further processing.” – Peter Malinowski
The nervous system is a dynamic entity, constantly changing and adapting to the environment. It will change size, activity, and connectivity in response to experience. These changes in the brain are called neuroplasticity. Over the last decade neuroscience has been studying the effects of contemplative practices on the brain and has identified neuroplastic changes in widespread area. and have found that meditation practice appears to mold and change the brain, producing psychological, physical, and spiritual benefits. These brain changes with mindfulness practice are important and need to be further investigates.
Meditation practice results in a shift in mental processing. It produces a reduction of mind wandering and self-referential thinking and an increase in attention and higher-level thinking. The neural system that underlies mind wandering is termed the Default Mode Network (DMN) and consists in a set of brain structures including medial prefrontal cortex, posterior cingulate, lateral temporal cortex and the hippocampus. The neural system that underlies attention and is termed the Dorsal Attentional Network (DAN). and includes the frontal eye fields and the areas around the precentral sulcus and intraparietal sulcus. It is possible, then, that meditation over time produces changes in these brain areas improving attentional ability.
In today’s Research News article “Attention and Default Mode Network Assessments of Meditation Experience during Active Cognition and Rest.” (See summary below or view the full text of the study at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8144977/ ) Devaney and colleagues recruited experienced meditators (average of 7 years of practice) and non-meditators matched on demographic variables. The participants performed attention tasks (multiple object tracking, a sustained attention task, and oddball tasks, a sustained spatial attention task) while having their brains scanned with functional Magnetic Resonance Imaging (fMRI).
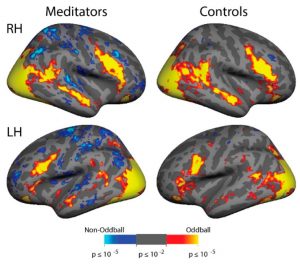
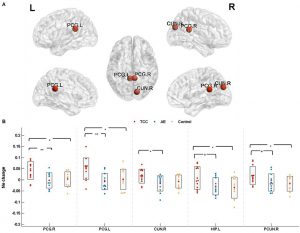
There were no significant differences between the experienced meditators and the matched controls in their performance of the attention tasks. But during the sustained attention task the meditators in comparison to the controls had increases in activation of the brain’s Dorsal Attentional Network at the same time as a significant decrease in the brain’s Default Mode Network. In addition, during the sustained attention task the meditators had significantly greater anticorrelations of activity between the two networks indicating higher levels of inhibitory activity between networks.
The Dorsal Attentional Network has been shown to be involved in focused attention. Hence, the results suggest that experience in meditation improves the response of the brain areas responsible for focused attention when needed. Alternatively, the Default Mode Network has been shown to be involved in mind wandering. Hence, the results suggest that experience in meditation reduces the response of the brain areas responsible a loss of focused attention and mind wandering when needed. Further, the results suggest that experience in meditation leads to a greater ability of the brain to focus attention while preventing mind wandering.
The fact that experienced meditators did not differ from controls in attentional task performance is a bit disappointing. But on average the meditators performed better but because of a small number of participants, the differences were not statistically significant. Perhaps with larger groups differences would be found. But the lack of statistical power makes the significant brain activation differences observed during sustained attention even more striking. This all suggests that meditation practice shapes the brain for better attentional ability.
So, meditation strengthens brain attentional network.
“Meditation is an important form of self-control and a healthy practice. It augments focus and attention and could be used to enhance empathy and all attentional capacities.” – Gabriel José Corrêa Mograbi
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Google+ https://plus.google.com/106784388191201299496/posts and on Twitter @MindfulResearch
Study Summary
Devaney, K.J.; Levin, E.J.; Tripathi, V.; Higgins, J.P.; Lazar, S.W.; Somers, D.C. Attention and Default Mode Network Assessments of Meditation Experience during Active Cognition and Rest. Brain Sci. 2021, 11, 566. https://doi.org/10.3390/ brainsci11050566
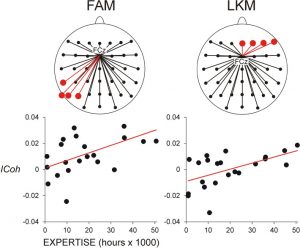
Abstract: Meditation experience has previously been shown to improve performance on behavioral assessments of attention, but the neural bases of this improvement are unknown. Two prominent, strongly competing networks exist in the human cortex: a dorsal attention network, that is activated during focused attention, and a default mode network, that is suppressed during attentionally demanding tasks. Prior studies suggest that strong anti-correlations between these networks indicate good brain health. In addition, a third network, a ventral attention network, serves as a “circuit-breaker” that transiently disrupts and redirects focused attention to permit salient stimuli to capture attention. Here, we used functional magnetic resonance imaging to contrast cortical network activation between experienced focused attention Vipassana meditators and matched controls. Participants performed two attention tasks during scanning: a sustained attention task and an attention-capture task. Meditators demonstrated increased magnitude of differential activation in the dorsal attention vs. default mode network in a sustained attention task, relative to controls. In contrast, there were no evident attention network differences between meditators and controls in an attentional reorienting paradigm. A resting state functional connectivity analysis revealed a greater magnitude of anticorrelation between dorsal attention and default mode networks in the meditators as compared to both our local control group and a n = 168 Human Connectome Project dataset. These results demonstrate, with both task- and rest-based fMRI data, increased stability in sustained attention processes without an associated attentional capture cost in meditators. Task and resting-state results, which revealed stronger anticorrelations between dorsal attention and default mode networks in experienced mediators than in controls, are consistent with a brain health benefit of long-term meditation practice.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8144977/