Meditation Increases Functional Connectivity of Brain Networks
By John M. de Castro, Ph.D.
“It seems the longer you do meditation, the better your brain will be at self-regulation,” – Bin He
Mindfulness training has been shown through extensive research to be effective in improving physical and psychological health and particularly with reducing the physical and psychological reactions to stress. There are a number of ways that meditation practices produce these benefits, including changes to the brain and physiology. The nervous system changes in response to how it is used and how it is stimulated in a process called neuroplasticity. Highly used areas grow in size, metabolism, and connectivity. Mindfulness practices in general are known to produce these kinds of changes in the structure and activity of the brain. There is little research, however, on how these changes develop with meditation.
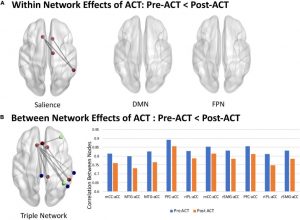
In today’s Research News article “Longitudinal effects of meditation on brain resting-state functional connectivity.” (See summary below or view the full text of the study at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8166909/ ) Zhang and colleagues recruited novice meditators enrolled in a university meditation course. They practiced focused attention meditation over 2 months twice a week in class and at home 5 times per week for 10 minutes. Before and after training the students had their brains scanned with functional Magnetic Resonance Imaging (f-MRI).
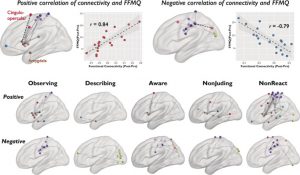
They found that after the 2-month meditation training the participants had significant increases in the functional connectivity within the Dorsal Attention Network of the brain and between the Dorsal Attention Network and the Default Mode Network and also between the Default Mode Network and the visual cortex.
The Dorsal Attention Network is a series of structures in the brain that are associated with attentional focusing while the Default Mode Network is a series of structures in the brain that are associated with self-referential thought and mind wandering. Typically, during focused attention meditation, particularly in novice meditators, the mind switches back and forth between focus on the object of meditation and unfocused mind wandering. During mind wandering, visualizations of this content often occur. This usually occurs repeatedly during the meditation session. This switching involves going back and forth between the Dorsal Attention Network and the Default Mode Network and the visual areas of the brain. The brain scan findings indicate that this results in an increase in the functional connectivity between the two networks. Hence, the changes in the mental contents during meditation are reflected in brain activity.
So, meditation increases functional connectivity of brain networks.
“So, not only did meditation change the structures in the participants’ brains, it also changed how they felt.” – Lela Moore
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Google+ https://plus.google.com/106784388191201299496/posts and on Twitter @MindfulResearch
Study Summary
Zhang, Z., Luh, W. M., Duan, W., Zhou, G. D., Weinschenk, G., Anderson, A. K., & Dai, W. (2021). Longitudinal effects of meditation on brain resting-state functional connectivity. Scientific reports, 11(1), 11361. https://doi.org/10.1038/s41598-021-90729-y
Abstract
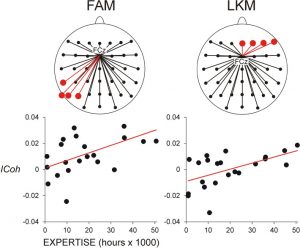
Changes in brain resting-state functional connectivity (rsFC) were investigated using a longitudinal design by following a 2-month focused attention meditation (FAM) practice and analyzing their association with FAM practice time. Ten novice meditators were recruited from a university meditation course. Participants were scanned with a resting-state fMRI sequence with multi-echo EPI acquisition at baseline and at the 2-month follow-up. Total FAM practice time was calculated from the daily log of the participants. We observed significantly increased rsFC between the posterior cingulate cortex (PCC) and dorsal attention network (DAN), the right middle temporal (RMT) region and default mode network (DMN), the left and right superior parietal lobules (LSPL/RSPL) and DMN, and the LSPL/RSPL and DAN. Furthermore, the rsFC between the LSPL and medial prefrontal cortex was significantly associated with the FAM practice time. These results demonstrate increased connectivity within the DAN, between the DMN and DAN, and between the DMN and visual cortex. These findings demonstrate that FAM can enhance the brain connection among and within brain networks, especially DMN and DAN, indicating potential effect of FAM on fast switching between mind wandering and focused attention and maintaining attention once in the attentive state.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8166909/