Mindfulness is Associated with Better Perinatal Mental Health Among Uncertainty Produced by Covid-19
By John M. de Castro, Ph.D.
“use of a mindfulness-based meditation app may benefit patients who are navigating the stressors of being pregnant during the COVID-19 pandemic.” – Orli K. Florsheim, MD
The period of pregnancy is a time of intense physiological and psychological change. Anxiety, depression, and fear are quite common during pregnancy. More than 20 percent of pregnant women have an anxiety disorder, depressive symptoms, or both during pregnancy. The psychological health of pregnant women has consequences for fetal development, birthing, and consequently, child outcomes. Depression during pregnancy is associated with premature delivery and low birth weight.
In addition, immediately after birth it is common for the mother to experience mood swings including what has been termed “baby blues,” a sadness that may last for as much as a couple of weeks. But some women experience a more intense and long-lasting negative mood called postpartum depression. This occurs usually 4-6 weeks after birth in about 15% of births; about 600,000 women in the U.S. every year. For 50% of the women the depression lasts for about a year while about 30% are still depressed 3 years later.
Hence, it is clear that there is a need for methods to treat depression, and anxiety during the perinatal period. Since the fetus can be negatively impacted by drugs, it would be preferable to find a treatment that did not require drugs. Mindfulness training has been shown to improve anxiety and depression normally and to relieve maternal anxiety and depression during pregnancy and to relieve postpartum depression.
The COVID-19 pandemic has challenged the mental and physical health of the population. It has created intense stress for everyone including women during the perinatal period. Mindfulness is known to decrease the psychological and physical responses to stress and to improve well-being during the perinatal period. So, mindfulness training may be helpful in coping with the mental and physical challenges during the perinatal period resulting from the COVID-19 pandemic.
In today’s Research News article “The Indirect Effect of Parental Intolerance of Uncertainty on Perinatal Mental Health via Mindfulness During COVID-19.” (See summary below or view the full text of the study at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8171361/ ) Sbrilli and colleagues recruited pregnant women or women who had given birth in the last 6 months during the Covid-19 pandemic. They were measured for Intolerance of uncertainty, mindfulness, and psychological symptoms, including anxiety, depression, and somatization.
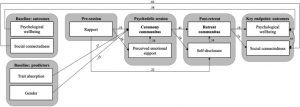
They performed a path analysis and found that in these perinatal women intolerance of uncertainty was associated with psychological symptoms, especially anxiety and depression, directly and also indirectly by being associated with lower mindfulness which was, in turn, associated with greater psychological symptoms. The mindfulness facets that were significant in the indirect path were acting with awareness, non-reactivity, and describing.
The present study is correlational and as such caution must be exercised in reaching causal conclusions. But mindfulness has been shown in prior research to produce reductions in anxiety and depression. So, reduced mindfulness in the present study was probably the cause of the increased psychological symptoms. What’s new here is the finding that intolerance of uncertainty is directly and through mindfulness indirectly associated with increased psychological symptoms in perinatal women.
Intolerance of uncertainty is a fear of the unknown. During Covid-19 this fear is greatly amplified and the present results suggest that this results in greater anxiety and depression in these women. But since mindfulness is an intermediary it is possible that improvements in mindfulness, perhaps through training, could intervene to block the effects of intolerance of uncertainty on psychological symptoms. This is supported by the findings that mindfulness during Covid-19 improves psychological well-being.
Anxiety and depression during pregnancy can affect the birth and condition of the newborn. In addition, after birth they can affect post-partum depression. So, improving mindfulness is important during the perinatal period to improve the health and well-being of the infant and the mother. This becomes more important during the pandemic where uncertainty can exacerbate anxiety and depression.
So, mindfulness is associated with better perinatal mental health among uncertainty produced by Covid-19.
“The strength of mediation habits may play a role in pregnant women’s mental health during COVID-19. Stronger meditation habits may prevent increases in stress despite increased worry related to getting infected by COVID-19 and may reduce symptoms of depression and PTSD.” – Jennifer Huberty
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are a also available on Google+ https://plus.google.com/106784388191201299496/posts and on Twitter @MindfulResearch
Study Summary
Sbrilli, M. D., Haigler, K., & Laurent, H. K. (2021). The Indirect Effect of Parental Intolerance of Uncertainty on Perinatal Mental Health via Mindfulness During COVID-19. Mindfulness, 1–10. Advance online publication. https://doi.org/10.1007/s12671-021-01657-x
Abstract
Objectives
The COVID-19 pandemic is associated with mental health difficulties, especially during pregnancy and early postpartum. Intolerance of uncertainty (IU) and reduced capacity for mindfulness—a protective factor for child-bearers—may be particularly relevant factors driving mental health problems given the unpredictable nature of the pandemic. The current study aims to shed light on modifiable paths to perinatal psychological distress by testing whether there is an indirect effect of IU on psychological symptoms through a perceived reduction in mindfulness during the pandemic.
Methods
Pregnant individuals (67%, n = 133) and new mothers within 6 months postpartum (33%, n = 66) participated in a cross-sectional online survey assessing IU, current and retrospective pre-pandemic mindfulness (FFMQ), and psychological symptoms (anxiety, depression, somatization; BSI). Perceived change in mindfulness was captured by including retrospective mindfulness as a covariate in the PROCESS macro used for analyses.
Results
Tests of the direct association between mindfulness, IU, and psychological symptoms showed significant effects of IU (b = 0.46, SE = 0.064; p < .001) and perceived decrease in mindfulness during the pandemic (b = − 0.72, SE = 0.08, p < .001) on psychological symptoms (R2 = .21–.34; F[2, 197] = 51.13–52.81, p < .001). The indirect effect of IU on symptoms via perceived decrease in mindfulness during the pandemic (b = 0.13, SE = 0.043, 95%CI [.060, .226]) was significant (R2 = .41, F[3, 195] = 45.08, p < .001).
Conclusions
Results suggest that mothers who are less able to tolerate uncertainty experience more psychological symptoms, in part due to perceived reduction in mindfulness during the pandemic. Future research should examine whether IU is a screening risk marker and target for mindfulness-based interventions to improve maternal well-being and family outcomes.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8171361/