Mindfulness Increases the Ability to Change Behavior for the Good
By John M. de Castro, Ph.D.
“Training your mind to be in the present moment is the #1 key to making healthier choices.” – Susan Albers
Many health problems are behavioral problems or have their origins in maladaptive behavior. This is evident in car accident injuries that are frequently due to behaviors, such as texting while driving, driving too fast or aggressively, or driving drunk. Other problematic behaviors are cigarette smoking, alcoholism, drug use, or unprotected sex. Problems can also be produced by lack of appropriate behavior such as sedentary lifestyle, not eating a healthy diet, not getting sufficient sleep or rest, or failing to take medications according to the physician’s orders.
Hence, promoting behavior change to healthy behaviors and eliminating unhealthy ones has the potential to markedly improve health. Mindfulness training has been shown to promote health and improve illness. It is well established that mindfulness can improve healthy behaviors. The research has been accumulating. So, it is reasonable to stop and summarize what has been learned.
In today’s Research News article “.” (See summary below or view the full text of the study at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7647439/ ) Schuman-Olivier and colleagues review and summarize the published research studies on the ability of mindfulness training to promote behavior change and also the mechanism by which this is accomplished..
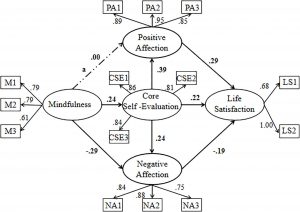
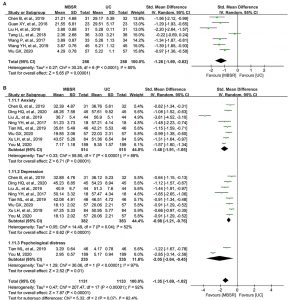
They summarize the research as demonstrating that mindfulness training improves self-regulation. This includes improvements in attention, cognitive control, emotion regulation, and self-related processes. These improvements in self-regulation results in an increased ability to change behavior from unhealthy behaviors to more healthy behaviors. This has been shown to be true with substance abuse, eating disorders, tobacco smoking, self-management with chronic diseases, violence, suicide, and self-harm.
They conclude that the published research supports the model that mindfulness training increases self-regulation which in turn supports behavior change.
“A mind set in its ways is wasted.” – Eric Schmidt
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Twitter @MindfulResearch
Study Summary
Schuman-Olivier Z, Trombka M, Lovas DA, Brewer JA, Vago DR, Gawande R, Dunne JP, Lazar SW, Loucks EB, Fulwiler C. Mindfulness and Behavior Change. Harv Rev Psychiatry. 2020 Nov/Dec;28(6):371-394. doi: 10.1097/HRP.0000000000000277. PMID: 33156156; PMCID: PMC7647439.
Abstract
Initiating and maintaining behavior change is key to the prevention and treatment of most preventable chronic medical and psychiatric illnesses. The cultivation of mindfulness, involving acceptance and nonjudgment of present-moment experience, often results in transformative health behavior change. Neural systems involved in motivation and learning have an important role to play. A theoretical model of mindfulness that integrates these mechanisms with the cognitive, emotional, and self-related processes commonly described, while applying an integrated model to health behavior change, is needed. This integrative review (1) defines mindfulness and describes the mindfulness-based intervention movement, (2) synthesizes the neuroscience of mindfulness and integrates motivation and learning mechanisms within a mindful self-regulation model for understanding the complex effects of mindfulness on behavior change, and (3) synthesizes current clinical research evaluating the effects of mindfulness-based interventions targeting health behaviors relevant to psychiatric care. The review provides insight into the limitations of current research and proposes potential mechanisms to be tested in future research and targeted in clinical practice to enhance the impact of mindfulness on behavior change.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7647439/