Improve Cognitive Flexibility with Mindful Non-Reactivity
By John M. de Castro, Ph.D.
“Mindfulness meditation practice and self-reported mindfulness were correlated directly with cognitive flexibility and attentional functioning.” – Daphne Davis
Mindfulness training has been shown to be effective in improving physical and psychological health and particularly with the physical and psychological reactions to stress. Mindfulness also decreases the individual’s tendency to use tried and true solutions to problems and thereby improves cognitive flexibility. This has led to an increasing adoption of these mindfulness techniques for the health and well-being of both healthy and ill individuals.
Mindfulness, however, is complex and includes facets such as observing, describing, non-reacting, non-judging, and acting with awareness. It is not known which of these facets or which combinations of facets are responsible for the beneficial effects of mindfulness including improved cognitive flexibility. Hence there is a need to investigate the facets of mindfulness and their relationship to the psychological flexibility of the participants.
In today’s Research News article “The Mediating Role of Non-reactivity to Mindfulness Training and Cognitive Flexibility: A Randomized Controlled Trial.” (See summary below or view the full text of the study at: https://www.frontiersin.org/articles/10.3389/fpsyg.2020.01053/full?utm_source=F-AAE&utm_medium=EMLF&utm_campaign=MRK_1365539_69_Psycho_20200630_arts_A), Zou and colleagues recruited online moderately stressed adults who did not have a mindfulness practice. They were matched and randomly assigned to a wait-list control condition or to receive a once a week for 2.5 hours for 8 weeks Mindfulness-Based Stress Reduction (MBSR) program. MBSR includes meditation, body scan, yoga practices, and discussion along with 45-minute daily home guided meditation practice. They were measured, before, twice during, and after training for mindfulness, including observing, describing, non-reacting, non-judging, and acting with awareness facets, cognitive flexibility, and perceived stress.
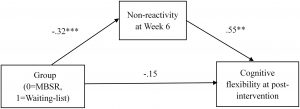
They found that in comparison to baseline and the wait-list control group, the group that received the Mindfulness-Based Stress Reduction (MBSR) program had significant increases in cognitive flexibility. A mediation analysis revealed that MBSR training solely indirectly by increasing the non-reactivity facet of mindfulness which in turn increased cognitive flexibility. Surprisingly, although perceived stress decreased over the 8-week period, there was no significant difference between groups.
Cognitive flexibility is ‘the ability to flexibly and adaptively respond to the environments, as opposed to the rigid or automatic thinking style, triggered by prior experience”. Non-reactivity involves allowing experiences to come and go without reacting in an effort to change them. By not reacting in an autonomic way, it opens up the ability to react flexibly and adaptively to the situation. This ability makes the individual better able to address events in their life and thereby improve their well- being.
So, improve cognitive flexibility with mindful non-reactivity.
“mindfulness involves cultivation of a “beginner’s mind”, and demonstrate that mindfulness practice reduces cognitive rigidity via the tendency to overlook simple novel solutions to a situation due to rigid and repetitive thought patterns formed through experience.” – Jonathan Greenberg
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Google+ https://plus.google.com/106784388191201299496/posts and on Twitter @MindfulResearch
Study Summary
Zou Y, Li P, Hofmann SG and Liu X (2020) The Mediating Role of Non-reactivity to Mindfulness Training and Cognitive Flexibility: A Randomized Controlled Trial. Front. Psychol. 11:1053. doi: 10.3389/fpsyg.2020.01053
Mindfulness training has been shown to have a beneficial effect on cognitive flexibility. However, little is known about the mediators that produce this effect. Cross-sectional studies show that there might be a link between Non-judgment, Non-reactivity and cognitive flexibility. Longitudinal studies examining whether Non-judgment or Non-reactivity mediate the effectiveness of mindfulness training on improving cognitive flexibility are lacking. The present study aims to test the effect of mindfulness training on increasing cognitive flexibility and to test whether this effect is mediated by Non-judgment or Non-reactivity. We conducted a single-blind randomized controlled trial in 54 nonclinical high-stress participants between October 2018 and January 2019. Participants were randomly assigned to a Mindfulness Based Stress Reduction (MBSR) group or a waitlist control group. The experimenters were blind to the group assignment of participants. The MBSR group received 8-weekly sessions (2.5-h per week) and a one-day retreat (6-h), and was required to accomplish a 45-min daily formal practice during the intervention. The waitlist control group did not receive any intervention during the waiting period and received a 2-day (6-h per day) mindfulness training after the post-intervention. The primary outcome was self-report cognitive flexibility and perceived stress administered before and after MBSR. The secondary outcome was self-report mindfulness skills (including Non-reactivity and Non-judgment) measured at pre-treatment, Week 3, Week 6, and post-intervention. For cognitive flexibility, mixed-model repeated-measure ANOVA results showed that there were significant main effects of Time, Group and a significant interaction of Time by Group. Follow-up ANOVA indicated that the MBSR group was associated with greater improvements in cognitive flexibility than the waitlist. Path analysis results showed that the effect of the treatment on cognitive flexibility at post-treatment was fully mediated by Non-reactivity at Week 6. The mediation effects of Non-reactivity at Week 3, and Non-judgment at Week 3 and Week 6 were not significant. Our findings support the efficacy of MBSR on improving cognitive flexibility. Non-reactivity is an important element of the effectiveness of MBSR training on cognitive flexibility.