“Migraine is a disorder of a hyper-excitable brain, and it makes sense for people with migraine to adopt a stress-reducing . . . One behavioral intervention that may be useful, not only for migraine, but also for life in general, is what is called mindfulness meditation.” – John Wendt
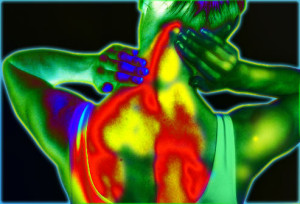
Migraine headaches are a torment far beyond the suffering of a common headache. It is an intense throbbing pain usually unilateral, focused on only one side of the head. They last from 4 hours to 3 days. They are actually a collection of neurological symptoms. Migraines often include: visual disturbances, nausea, vomiting, dizziness, extreme sensitivity to sound, light, touch and smell, and tingling or numbness in the extremities or face. Migraines are the 8th most disabling illness in the world. They disproportionately affect women with about 18% of American women and 6% of men suffering from migraine. In the U.S. they affect roughly 40 million men, women and children. While most sufferers experience attacks once or twice a month, 14 million people or about 4% have chronic daily headaches. Migraines are very disruptive to the sufferer’s personal and work lives as most people are unable to work or function normally when experiencing a migraine.
There is no known cure for migraine headaches. Treatments are targeted at managing the symptoms. Prescription and over-the-counter pain relievers are frequently used. There are a number of drug and drug combinations that appear to reduce the frequency of migraine attacks. These vary in effectiveness but unfortunately can have troubling side effects and some are addictive. Behaviorally, relaxation and sleep appear to help lower the frequency of migraines. Mindfulness practices have been shown to reduce stress and improve relaxation (see http://contemplative-studies.org/wp/index.php/category/research-news/stress/). So, they may be useful in preventing migraines. Indeed, it has been shown that Mindfulness Based Stress reduction (MBSR) practice can reduce tension headache pain (see http://contemplative-studies.org/wp/index.php/2015/09/07/headaches-are-a-headache-reduce-them-with-mindfulness/).
Wachholtz and colleagues have previously shown that adding a spiritual dimension to meditation can increase the effectiveness of meditation for increasing pain tolerance. In today’s Research News article “Effect of Different Meditation Types on Migraine Headache Medication Use”
Wachholtz and colleagues randomly assigned migraine sufferers to four conditions, spiritual meditation, internal secular meditation, external secular meditation, and progressive muscle relaxation. The differences between the meditation groups was solely a phrase that the participants were asked to repeat a few times at the beginning of the meditation. The phrases were for spiritual meditation, “God is peace,” “God is joy,” God is good,” and “God is love,” or alternatively substituting the words “Mother Nature” for God; internal secular meditation, “I am content,” “I am joyful,” “I am good,” “I am happy;” and for external secular meditation, “Grass is green,” “Sand is soft,” “Cotton is fluffy,” “Cloth is smooth.” Practice continued 20 minutes once a day for 30 days.
They found that over the 30 days of practice all groups had a decrease in the frequency of migraines and the amounts of pain medications taken, but the spiritual meditation group had a significantly greater decrease in frequency and medication use than the other three groups. None of the treatments appeared to change the severity of the migraines. Hence, adding the spiritual dimension to the meditation enhanced its effectiveness with migraines. Unfortunately, once a migraine began, nothing altered its magnitude or duration.
There is evidence that meditation can reduce pain (see http://contemplative-studies.org/wp/index.php/category/research-news/pain/). But, it is not known how the addition of simple spiritual phrases at the beginning of the meditation might improve its effectiveness. It is possible that the spiritual phrases were more effective than the secular phrases in focusing attention for the meditation session and thereby making it more effective. It is also possible that the phrases increased the individual’s ability to let go of struggling by turning over responsibility to a higher power. But, these are pure speculations. It will take further research to clarify the mechanism of action. But, it is clear that adding a spiritual dimension to meditation increases its effectiveness against migraine headaches.
So, add spirituality to meditation and improve migraines.
“although mindfulness is often thought of as a method of spiritual enlightenment, the underlying principles for healing are based on science. In a nutshell, mindfulness is capable of changing our brain chemistry, which impacts each and every one of our systems and organs.” – Cynthia Perkins
CMCS – Center for Mindfulness and Contemplative Studies