By John M. de Castro, Ph.D.
“With mindfulness, we learn to truly stand in our own shoes. From this perspective, mindfulness is a practice of self–empathy. This kind of self-awareness allows us to develop empathic connections to others. As we experience the landscape of our inner life with more detail and richness, our ability to understand the inner lives of others expands.” – Matthew Brensilver
Humans are social animals. This is a great asset for the species as the effort of the individual is amplified by cooperation. In primitive times, this cooperation was essential for survival. But in modern times it is also essential, not for survival but rather for making a living and for the happiness of the individual. This ability to cooperate is so essential to human flourishing that it is built deep into our DNA and is reflected in the structure of the human nervous system.
This cooperation is reflected in the modern workplace where the enterprise is founded on a large number of employees each playing their individual role in the totality of the business. Complex organizations such as modern corporations produce interpersonal challenges and stresses on the individual. Fortunately, the human has considerable social skills including the abilities to be compassionate and understanding of others, helping to cope with these challenges. This involves a considerable ability to regulate emotions, to not react to the individual’s momentary emotions to consider the greater good.
Mindfulness may be of great assistance. It is known to produce better emotion regulation and to promote compassion and empathy. Hence, mindfulness improves the individual’s ability to work cooperatively with others. As a result, mindfulness training has been shown to improve performance and satisfaction in the workplace. In today’s Research News article “Mindfulness training increases cooperative decision making in economic exchanges: Evidence from fMRI.” See:
or below, Kirk and colleagues explore the effects of mindfulness training on economic cooperation and the underlying neural systems. They recruited adults to participate in a stress reduction program. They were randomly assigned either to an 8-week Mindfulness Based Stress Reduction (MBSR) program or an 8-week progressive muscle relaxation program. All participants were measured before and after training for mindfulness and mood states. They also played an “Ultimatum Game” in which they were asked to accept or reject offers of splits of $20 all of which produced a gain for participants but varied in fairness of the split. Surprisingly participants frequently reject unfair offers even when it is in their best interest to accept all non-zero offers. Finally, participants’ brains were scanned with functional Magnetic Resonance Imaging (fMRI) while playing the game.
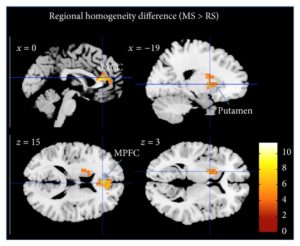
They found that mindfulness training significantly increased the acceptance of splits particularly with the most unfair but profitable splits, increasing from 24% to 44% after training. This resulted in a significant increase in the total distribution of money to both the participant and their supposed partner. Hence, mindfulness training produced greater profit for both. There was no change for the relaxation group. Both groups increased in mindfulness and the greater the increase in mindfulness, the greater the acceptance rates of the offers. In terms of the nervous system activity they found that pre-training unfair offers led to increased activity of the Insula, but this activity was lower after mindfulness training. In addition, in the mindfulness trained participants, cooperation led to increased activity of the Septum. Mindfulness training was also found to increase the functional connectivity between the Insula and the Septum.
These results suggest that mindfulness training produces greater cooperation to the benefit of all participants and that these changes are reflected in changes in neural processing. Why would mindfulness training increase cooperation in the “Ultimatum Game.” Rejecting any off in the game actually reduces the gain for everyone including the participant. So, it is an irrational action. The offers that are rejected are those that are seen to gain more for another than the participant, to be unfair. So, it is this emotional reaction to the perceived unfairness that prompts the counterproductive action of rejecting the offer. Mindfulness training is known to improve emotion regulation, making the individual better able to respond adaptively to emotions. This is probably what made the mindfulness trained group better at cooperation in the face of perceived unfairness, responding rationally and adaptively, increasing profit for all. These effects of mindfulness training are reflected in changes in the brain.
So, build a cooperative brain with mindfulness.
“We are emotional beings and we can’t help but be affected by the varying moods and interactions we have with others. Life is always changing and this constant change can create difficult thoughts and emotions, which can flow into the workplace. The silver lining is that if we can meet suffering at work with concern and care, compassion naturally arises. Work environments that cultivate compassion create a much more positive and productive place to work.” – Carley Hauck
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Google+ https://plus.google.com/106784388191201299496/posts
Study Summary
Kirk U, Gu X, Sharp C, Hula A, Fonagy P, Montague PR. Mindfulness training increases cooperative decision making in economic exchanges: Evidence from fMRI. Neuroimage. 2016 Jun 4. pii: S1053-8119(16)30189-6. doi: 10.1016/j.neuroimage.2016.05.075
Abstract
Emotions have been shown to exert influences on decision making during economic exchanges. Here we investigate the underlying neural mechanisms of a training regimen which is hypothesized to promote emotional awareness, specifically mindfulness training (MT). We test the hypothesis that MT increases cooperative economic decision making using fMRI in a randomized longitudinal design involving 8 weeks of either MT or active control training (CT). We find that MT results in an increased willingness to cooperate indexed by higher acceptance rates to unfair monetary offers in the Ultimatum Game. While controlling for acceptance rates of monetary offers between intervention groups, subjects in the MT and CT groups show differential brain activation patterns. Specifically, a subset of more cooperative MT subjects displays increased activation in the septal region, an area linked to social attachment, which may drive the increased willingness to express cooperative behavior in the MT cohort. Furthermore, MT resulted in attenuated activity in anterior insula compared with the CT group in response to unfair monetary offers post-training, which may suggest that MT enables greater ability to effectively regulate the anterior insula and thereby promotes social cooperation. Finally, functional connectivity analyses show a coupling between the septal region and posterior insula in the MT group, suggesting an integration of interoceptive inputs. Together, these results highlight that MT may be employed in contexts where emotional regulation is required to promote social cooperation.