By John M. de Castro, Ph.D.
“Our minds wander, on average 50 percent of the time. The exact rate varies enormously. . . . Noticing where your mind has gone – checking your twitter feed instead of working on that report – gives you the chance for a second thought: “my mind has wandered off again.” That very thought disengages your brain from where it has wandered and activates brain circuits that can help your attention get unstuck and return to the work at hand.” – Daniel Goleman
We spend a tremendous amount of our time with our minds wandering and not on the task or the environment at hand. We daydream, plan for the future, review the past, ruminate on our failures, exalt in our successes. In fact, we spend almost half of our waking hours off task with our mind wandering. You’d think that if we spend so much time doing this it must be enjoyable. But, in fact research has shown that when our mind is wandering we are actually unhappier than when we are paying attention to what is at hand.
A system of the brain known as the Default Mode Network (DMN) becomes active during wind wandering and relatively quiet during focused on task behavior. It is involved when we are engaged in internally focused tasks such as recalling deeply personal memories, daydreaming, sleeping, imagining the future and trying to take the perspective of others. The DMN involves neural structures including the medial prefrontal cortex, anterior and posterior cingulate cortices, precuneus, inferior parietal cortex, and lateral temporal cortex. These areas of the DMN are functionally connected, such that they are simultaneously active during mind wandering.
Meditation is known to reduce the size and activity of the Default Mode Network (DMN) through a process known as neuroplasticity where the size and connectivity of neural structures are modified by experience. In addition, meditation appears to decrease the functional connectivity of these structures. The research underlying these conclusions, however, suffer from a flaw in that meditation is compared to rest or to non-meditators. It is possible that any active mental task could also have the same effects on the DMN. There is thus a need to investigate the differences between the effects of meditation and other active mental activities on the activity of the DMN.
In today’s Research News article “Meditation leads to reduced default mode network activity beyond an active task.” See:
or see summary below or view the full text of the study at:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4529365/
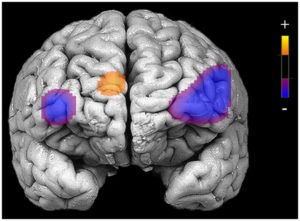
Garrison and colleagues recruited experienced meditators and non-meditators and scanned their brains (functional Magnetic Imaging, fMRI) while they either followed meditation instructions or an active mental task, making decisions as to whether adjectives applied to the self or to case. As expected the meditators reported less mind wandering during meditation. Importantly, they found that the meditators had significantly lower activity in the Default Mode Network (DMN) than the controls during the meditations but not during the active task.
These findings are important in that they demonstrate that the reduction in the DMN activity is not due to just any active mental task but specifically to meditation. The results also replicate the finding that meditation lowers mind wandering and the activity of the DMN. Hence meditation in particular appears to have the ability to reduce mind wandering, improving focus, by decreasing the activity of the brain system responsible for mind wandering.
So, reduce brain induced mind wandering with meditation.
“new knowledge about the default mode network and the self-reflecting thoughts that it stimulates may facilitate our understanding of how we function in our daily lives. We are more than intellect or the motor control of arms and legs, which is often the focus of brain researchers. Perhaps it may at times be good to know that our brain actually gives us room for our spontaneous thoughts and the associations and emotions that may at first seem a bit weird.” – Marcus Raichle
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Google+ https://plus.google.com/106784388191201299496/posts
Study Summary
Garrison, K. A., Zeffiro, T. A., Scheinost, D., Constable, R. T., & Brewer, J. A. (2015). Meditation leads to reduced default mode network activity beyond an active task. Cognitive, Affective & Behavioral Neuroscience, 15(3), 712–720. http://doi.org/10.3758/s13415-015-0358-3
Abstract
Meditation has been associated with relatively reduced activity in the default mode network, a brain network implicated in self-related thinking and mind wandering. However, previous imaging studies have typically compared meditation to rest despite other studies reporting differences in brain activation patterns between meditators and controls at rest. Moreover, rest is associated with a range of brain activation patterns across individuals that has only recently begun to be better characterized. Therefore, this study compared meditation to another active cognitive task, both to replicate findings that meditation is associated with relatively reduced default mode network activity, and to extend these findings by testing whether default mode activity was reduced during meditation beyond the typical reductions observed during effortful tasks. In addition, prior studies have used small groups, whereas the current study tested these hypotheses in a larger group. Results indicate that meditation is associated with reduced activations in the default mode network relative to an active task in meditators compared to controls. Regions of the default mode showing a group by task interaction include the posterior cingulate/precuneus and anterior cingulate cortex. These findings replicate and extend prior work indicating that suppression of default mode processing may represent a central neural process in long-term meditation, and suggest that meditation leads to relatively reduced default mode processing beyond that observed during another active cognitive task.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4529365/