Meditation Comes in Seven Different Varieties
By John M. de Castro, Ph.D.
“Experienced meditators agree: a daily meditation practice can have significant benefits for mental and physical health. But one thing they probably won’t agree on? The most effective types of meditation. That’s simply because it’s different for everyone. After all, there are literally hundreds of meditation techniques encompassing practices from different traditions, cultures, spiritual disciplines, and religions.” Headspace
Meditation training has been shown to improve health and well-being. It has also been found to be effective for a large array of medical and psychiatric conditions, either stand-alone or in combination with more traditional therapies. As a result, meditation training has been called the third wave of therapies. One problem with understanding meditation effects is that there are, a wide variety of meditation techniques and it is not known which work best for improving different conditions.
There are a number of different types of meditation. Classically they’ve been characterized on a continuum with the degree and type of attentional focus. In focused attention meditation, the individual practices paying attention to a single meditation object. Transcendental meditation is a silent mantra-based focused meditation in which a word or phrase is repeated over and over again. In open monitoring meditation, the individual opens up awareness to everything that’s being experienced regardless of its origin. In Loving Kindness Meditation the individual systematically pictures different individuals from self, to close friends, to enemies and wishes them happiness, well-being, safety, peace, and ease of well-being.
But there are a number of techniques that do not fall into these categories and even within these categories there are a number of large variations. In today’s Research News article “What Is Meditation? Proposing an Empirically Derived Classification System.” (See summary below or view the full text of the study at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6803504/), Matko and colleagues attempt to develop a more comprehensive system of classification. They found 309 different techniques but reduced them down to the 20 most popular ones. They recruited 100 meditators with at least 2 years of experience and asked them to rate how similar each technique was to every other technique.
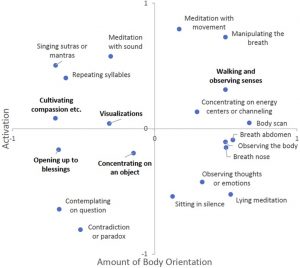
They applied multidimensional scaling to the data which uncovered two dimensions that adequately described all of the 20 techniques. The analysis revealed a dimension of the amount of activation involved and a dimension of the amount of body orientation involved. All 20 techniques were classified within these two dimensions. Visual inspection of where the various techniques fell on the two dimensions produces 7 different clusters labelled as “(1) Body-centered meditation, (2) mindful observation, (3) contemplation, (4) mantra meditation, (5) visual concentration, (6) affect-centered meditation, and (7) meditation with movement.”
Within the high activation and low body orientation quadrant there was one cluster identified, labelled “Mantra Meditation” including singing sutras/mantras/invocations, repeating syllables and meditation with sounds. Within the low activation and low body orientation quadrant there were three clusters identified, labelled “affect-centered meditation” including cultivating compassion and opening up to blessings; “visual orientations” including visualizations and concentrating on an object; and “contemplation” including contemplating on a question and contradictions or paradoxes.
Within the high activation and high body orientation quadrant there was one cluster identified, labelled “meditation with movement” including “meditation with movement, manipulating the breath, and walking and observing senses. Within the low activation and high body orientation quadrant there was one cluster identified, labelled “mindful observation” including observing thoughts, lying meditation, and sitting in silence. Finally, they identified a cluster with high body but straddling the activation dimension, labelled “body centered meditation” including concentrating on a energy centers or channeling, body scan, abdominal breath, nostril breath, and observing the body.
This 7-category classification system is interesting and based upon the ratings of experienced meditators. So, there is reason to believe that there is a degree of validity. In addition, the system is able to encompass 20 different popular meditation techniques. It remains for future research to investigate whether this classification system is useful in better understanding the effects of meditation or the underlying brain systems.
“Not all meditation styles are right for everyone. These practices require different skills and mindsets. How do you know which practice is right for you? “It’s what feels comfortable and what you feel encouraged to practice,” – Mira Dessy
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Google+ https://plus.google.com/106784388191201299496/posts and on Twitter @MindfulResearch
Study Summary
Matko, K., & Sedlmeier, P. (2019). What Is Meditation? Proposing an Empirically Derived Classification System. Frontiers in psychology, 10, 2276. doi:10.3389/fpsyg.2019.02276
Abstract
Meditation is an umbrella term, which subsumes a huge number of diverse practices. It is still unclear how these practices can be classified in a reasonable way. Earlier proposals have struggled to do justice to the diversity of meditation techniques. To help in solving this issue, we used a novel bottom-up procedure to develop a comprehensive classification system for meditation techniques. In previous studies, we reduced 309 initially identified techniques to the 20 most popular ones. In the present study, 100 experienced meditators were asked to rate the similarity of the selected 20 techniques. Using multidimensional scaling, we found two orthogonal dimensions along which meditation techniques could be classified: activation and amount of body orientation. These dimensions emphasize the role of embodied cognition in meditation. Within these two dimensions, seven main clusters emerged: mindful observation, body-centered meditation, visual concentration, contemplation, affect-centered meditation, mantra meditation, and meditation with movement. We conclude there is no “meditation” as such, but there are rather different groups of techniques that might exert diverse effects. These groups call into question the common division into “focused attention” and “open-monitoring” practices. We propose a new embodied classification system and encourage researchers to evaluate this classification system through comparative studies.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6803504/