Mindfulness Changes Neural Activity and Improves Major Depressive Disorder
By John M. de Castro, Ph.D.
“People at risk for depression are dealing with a lot of negative thoughts, feelings and beliefs about themselves and this can easily slide into a depressive relapse. . . MBCT helps them to recognize that’s happening, engage with it in a different way and respond to it with equanimity and compassion.” – Willem Kuyken
Clinically diagnosed depression is the most common mental illness, affecting over 6% of the population. Major depression can be quite debilitating. Depression can be difficult to treat and is usually treated with anti-depressive medication. But, of patients treated initially with drugs only about a third attained remission of the depression. After repeated and varied treatments including drugs, therapy, exercise etc. only about two thirds of patients attained remission. But drugs often have troubling side effects and can lose effectiveness over time. In addition, many patients who achieve remission have relapses and recurrences of the depression. Even after remission some symptoms of depression may still be present (residual symptoms).
Being depressed and not responding to treatment or relapsing is a terribly difficult situation. The patients are suffering and nothing appears to work to relieve their intense depression. Suicide becomes a real possibility. So, it is imperative that other treatments be identified that can relieve the suffering. Mindfulness training has been shown to be an effective treatment for depression and its recurrence and even in the cases where drugs fail.
The most commonly used mindfulness technique for the treatment of depression is Mindfulness-Based Cognitive Therapy (MBCT). MBCT involves mindfulness training, containing sitting and walking meditation and body scan, and cognitive therapy to alter how the patient relates to the thought processes that often underlie and exacerbate psychological symptoms. MBCT has been shown to be as effective as antidepressant drugs in relieving the symptoms of depression and preventing depression reoccurrence and relapse. In addition, it appears to be effective as either a supplement to or a replacement for these drugs. It is not known how MBCT produces its effects on major depression.
One way to observe the effects of MBCT on neural activity is to measure changes in the electroencephalogram (EEG), the rhythmic electrical activity that can be recorded from the scalp. The recorded activity can be separated into frequency bands. Delta activity consists of oscillations in the 0.5-3 cycles per second band. Theta activity in the EEG consists of oscillations in the 4-8 cycles per second band. Alpha activity consists of oscillations in the 8-12 cycles per second band. Beta activity consists of oscillations in the 15-25 cycles per second band while Gamma activity occurs in the 35-45 cycles per second band. Changes in these brain activities can be compared during different depths of meditation.
In today’s Research News article “Mindfulness-Based Cognitive Therapy in Recurrent MDD Patients With Residual Symptoms: Alterations in Resting-State Theta Oscillation Dynamics Associated With Changes in Depression and Rumination.” (See summary below or view the full text of the study at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8936084/ ) Wang and colleagues recruited patients with major depressive disorder being treated with drugs but with residual symptoms. They were provided with an 8-week program of Mindfulness-Based Cognitive Therapy (MBCT). Before and after training they were measured for mindfulness, depression, and rumination and had their resting state electroencephalogram (EEG) recorded.
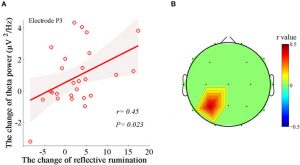
After completing Mindfulness-Based Cognitive Therapy (MBCT) there were significant reductions in depression which produced an 88% remission rate. There were also significant increases in mindfulness and reductions in brooding rumination. In addition, there was a significant increase in the theta rhythm power in the electroencephalogram (EEG). Finally, the greater the increase in theta power the greater the reductions in depression and rumination.
Hence, they found that Mindfulness-Based Cognitive Therapy (MBCT) is effective in treating depression even in patients under treatment with drugs. They also found that these improvements were related to increased theta power in the electroencephalogram (EEG). So, MBCT appears to change brain activity along with depression. The changes in the neural activity may be a mechanism by which MBCT helps improve depression symptoms.
“mindfulness is added to the standard depression treatment protocols, relapse rates decline.” – Sara Altshul
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Twitter @MindfulResearch
Study Summary
Wang, J., Ren, F., Gao, B., & Yu, X. (2022). Mindfulness-Based Cognitive Therapy in Recurrent MDD Patients With Residual Symptoms: Alterations in Resting-State Theta Oscillation Dynamics Associated With Changes in Depression and Rumination. Frontiers in psychiatry, 13, 818298. https://doi.org/10.3389/fpsyt.2022.818298
Abstract
Many patients with major depressive disorder (MDD) suffer from residual symptoms. Rumination is a specific known risk factor for the onset, severity, prolongation, and relapse of MDD. This study aimed to examine the efficacy and EEG substrates of mindfulness-based cognitive therapy (MBCT) in alleviating depression and rumination in an MDD population with residual symptoms. We recruited 26 recurrent MDD individuals who had residual symptoms with their current antidepressants to participate in the 8-week MBCT intervention. We evaluated the efficacy and changes in the dynamics of resting-state theta rhythm after the intervention, as well as the associations between theta alterations and improvements in depression and rumination. The participants showed reduced depression, enhanced adaptive reflective rumination, and increased theta power and phase synchronization after MBCT. The increased theta-band phase synchronizations between the right occipital regions and the right prefrontal, central, and parietal regions were associated with reduced depression, while the increase in theta power in the left parietal region was associated with improvements in reflective rumination. MBCT could alleviate depression and enhance adaptive, reflective rumination in recurrent MDD individuals with residual symptoms through the modulation of theta dynamics in specific brain regions.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8936084/