What’s Wrong with Meditation II – Improper Instruction
By John M. de Castro, Ph.D.
“The next biggest danger is that no one thinks there are or can be any dangers to meditation, so there is almost no discussion and information-gathering on the subject. Everyone is just going blah blah about the benefits. As a consequence, meditators are constantly being blindsided and derailed by things that should be trivial hazards, easily dismissed or bypassed. If we compare meditation to a day at the beach, it is as if people are saying, “Oh, don’t worry, you can never get enough direct sunlight. Just soak it up. You don’t even need a hat. And swim out in the ocean as far as you want. It’s a lake. With dolphins that will love you.”” – Lorin Roche
As was discussed in the prior essay on What’s Wrong with Meditation I – Expectations there are three essential problems with the way meditation has been presented in the west that have produced problems, misconceptions, and misunderstandings. First, meditation has been presented in a way that has evoked beliefs, ideas, and images that are overly idealized and not reflective of the typical experiences of meditation practice. Secondly, is the focus of the present essay, that immediately jumping into meditation practice has been encouraged, without the provision for proper background information, study, or instruction. Lastly, the jargon used to describe the process, experiences, obstacles, and results is extreme, evoking images and expectations that far exceed normal experience.
The Dalai Lama was brought on a tour of a major new meditation center in the United States. At the end of the tour, he simply asked “where’s the library?” He was astonished when he was told that there wasn’t one. He commented that before any of his new monks were allowed to meditate that had to spend at least a couple of years studying before they were allowed to meditate. He stressed that it is imperative that the practitioner have a proper background to understand the practical and theoretical basis for meditation before starting. This story exemplifies the difference between ancient Tibetan practice and meditation as it’s taught in the west where practitioners are launched into meditation practice with only minimal instruction. Hence people dive in without knowledge of obstacles and dangers hidden beneath the surface.
This western practice would be fine if meditation was straightforward and there weren’t any difficulties and traps that could ensnare the meditator. But, meditation practice is not simple and straightforward and without instruction in what to expect and how to recognize true progress, the practitioner is left to grope and stumble their way through the process. Beginners are generally not instructed, except in very general terms, as to what is the goal and how to recognize it if they attain it. They are frequently told to just follow and/or count the breath but receive no instruction as to what to do when their mind inevitably wanders. They are told simply return to following the breath. This was exactly how I was instructed when I began meditation practice.
As a result of this lack of instruction, beginners deride themselves for mind wandering making the process unpleasant. They are not told that this is effectively punishing themselves for recognizing that their mind has wandered. This makes it less likely that the individual will recognize and return from mental discursions. With a little instruction, they can learn that minds do what minds do, and that’s OK. They’re going to wander. Get used to it! But, they also need to be instructed to celebrate their recognizing it and returning to the meditative focus. This instruction produces reward for recognizing that the mind has wandered making it more likely that it will be recognized again and sooner. If beginners were simply given this much simple instruction their meditation practice will be much more enjoyable and productive and they’ll be much less likely to give up the practice.
Beginning meditators are frequently told that they should quiet the mind but are never instructed as to exactly what that means. They often confuse a quiet mind with a total blank, believing that a quiet mind is one without content. If they are simply instructed that they are to quiet the internal chatter, not everything. There’ll still be sounds, sights, odors, touches, etc. But when the mind is quiet there is no verbal commentary accompanying them. They are simply observing these stimuli as they are without categorization, judgment, labelling, reflection on past stimuli, or projections as to the future course of the stimuli. That’s a quiet mind. But few beginners are taught this. A completely blank mind can and will happen later in practice, but only after the mind has been quieted, not stopped. If beginning meditators were simply provided instruction about what is their goal and what a quiet mind is actually like their meditation practice will be much more enjoyable and productive.
A very important instruction for beginners is to warn them about the troubling kinds of thoughts and memories that often spontaneously arise during meditation. People come with the misconception that meditation will help them escape from their problems. Nothing could be further from the truth. In fact, meditation does the exact opposite, forcing the meditator to confront their issues. The strength here is that meditation is a wonderful occasion to begin to deal with these issues. But, often the thoughts or memories are overwhelming. Proper instruction is needed on how to work with issues gradually, avoiding delving too deeply too soon. At retreats, there are always boxes and boxes of tissues available for the inevitable copious tears shed by some of the participants as they are dealing with deeply troubling issues. Yes, in meditation you try to quiet the mind. But, in that relaxed quiet state, powerful, highly emotionally charged thoughts and memories are likely to emerge. The practitioner needs proper instruction beforehand of the likelihood of this happening and how to deal effectively with it. Knowing that this is normal, healthy, and part of the process, helps immeasurably to lessen the impact of these thoughts and memories on the individual and increases the likelihood that they can be effectively resolved. At times, professional therapeutic intervention may be needed. Once again, if this is understood ahead of time, the individual is more likely to seek assistance.
Meditation practice can also produce some troubling experiences beyond unmasking deep psychological issues. These are rarely presented or discussed with people before engaging in meditation. Not the least of these experiences are awakening experiences themselves. These can occur at any time and even to beginners. If they are not properly understood, they can lead to sometimes devastating consequences. These experiences are so powerful and unusual that they can be misinterpreted. Awakening experiences have been misdiagnosed as psychotic breaks and the individual placed on powerful drugs and/or institutionalized. There are no systematic studies of the extent of this problem, but a number of psychiatrists who meditate and understand awakening experiences have said that it is quiet extensive. At the very least, the individual may believe that they are losing their sanity or as one has said, “I just got used to the idea that occasionally I would have just one of those days.” This is one of the reasons why the Dalai Lama insists that beginners study first, so they can recognize what is happening to them if and when these experiences arise.
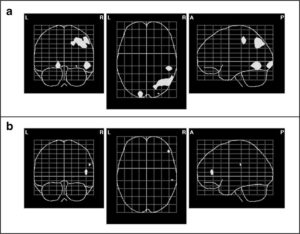
Meditation practice can sometimes produce energetic states that can vary in intensity, location, and duration. If and when these occur, they are usually quite surprising and unexpected. Many practitioners never experience these states or only experience very mild energy states. But, for those that do, if they have no prior instruction they can readily misinterpret them. They are sometimes called Kundalini energy states and involve energy focused in specific parts of the body or overall. They can feel like nervousness, tension, or almost like electrical currents flowing through the body and can produce spontaneous and undirected movements. These can be minor or overwhelmingly intense and can last from a few days to years. With these states sleep can be quite difficult and the individual may go days at a time without any sleep whatsoever. These energy states are usually found to be aversive and difficult to cope with. If the practitioner hasn’t been instructed about these states, they may seek out medical help. Unfortunately, the medical professions are not trained to recognize these states and often prescribe powerful anxiolytic drugs that can stupefy the individual but not affect the energies. Monasteries and major retreat centers are often equipped to recognize and treat these energies states. But, the vast majority of meditators and meditation instructions are completely devoid of an understanding of Kundalini energies. A little prior study and instruction can go a long way toward preventing misinterpretations and getting assistance from experienced teachers.
Another state that can be produced by awakening experiences has been termed as the “dark night of the soul.” After awakening there is, almost inevitably, a honeymoon period of happiness and bliss. But this is frequently followed by an aversive state that has been described as a spiritual desert. These have been reported by awakened individuals throughout the centuries, including the Christian and Sufi mystics and saints, Buddhist masters, and everyday practitioners. In these states the individual loses interest in life and seemingly has no motivation to do virtually anything. They feel emotionally dry and lament the loss of what they call the juice of life. Everything is flat and the individual often becomes deeply depressed. This dark night can last for months or years. To deal with dark nights the individual needs sophisticated instruction from accomplished teachers. No preparatory instruction will help to stop or prevent this from occurring. But, with proper instruction the individual can be better prepared to understand what is happening to them and what to expect in the future. This again can prevent misinterpretation and consequent maladaptive responses and harmful consequences.
At this point it should be clear why the Dalai Lama is so insistent upon extensive study and instruction prior to engaging in meditation. It can prevent potential negative reactions and consequences to some of the unexpected consequences of meditation. It has been my experience that the less instruction a person has prior to engaging in meditation the greater the likelihood that problems occur and the greater the likelihood of them being misinterpreted and counterproductive and even damaging responses occurring. So, study about meditation, work with an experienced teacher, and prepare yourself ahead of time before getting deeply involved in meditation practice. If you do, the rewards can be maximized and the pitfalls minimized, making practice productive and potentially profoundly altering.
The issues discussed above can seem off putting. You may be asking yourself if it makes any sense at all to engage in a meditation practice with all these potential problems. The answer is a resounding yes. The amazing benefits of meditation practice on your psychological, emotional, physical, and spiritual health make it well worth the effort. In fact, it has the potential to change you in profound ways for all of existence. The above caveats should be taken as indicators that study and guidance should be undertaken and that meditation should be practiced with understanding of what to expect both good and bad ahead of time. These warnings are important but should not be taken a stop signs, only caution signs. Know what you’re getting into, be prepared, and then reap the extraordinary benefits.
“It’s a kind of re-birth. The dark night of the soul is a kind of death that you die. What dies is the egoic sense of self. Of course, death is always painful, but nothing real has actually died there – only an illusory identity. Now it is probably the case that some people who’ve gone through this transformation realized that they had to go through that, in order to bring about a spiritual awakening. Often it is part of the awakening process, the death of the old self and the birth of the true self.” – Eckhart Tolle
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Google+ https://plus.google.com/106784388191201299496/posts and on Twitter @MindfulResearch