By John M. de Castro, Ph.D.
“Meditation isn’t a magic bullet for depression, as no treatment is, but it’s one of the tools that may help manage symptoms.” – Alice Walton
Depression is the most common mental illness affecting over 6% of the population. It is debilitating by producing any or all of a long list of symptoms including: feelings of sadness or unhappiness, change in appetite or weight, slowed thinking or speech, loss of interest in activities or social gatherings, fatigue, loss in energy, sleeplessness, feelings of guilt or anger over past failures, trouble concentrating, indecisiveness, anger or frustration for no distinct reason, thoughts of dying, death and suicide. The first line treatment is antidepressant drugs. But, depression can be difficult to treat. Of patients treated initially with drugs only about a third attained remission of the depression. After repeated and varied treatments including drugs, therapy, exercise etc. only about two thirds of patients attained remission. This leaves a third of all patients treated without success.
Mindfulness practices have been demonstrated to be beneficial for depression. They not only reduce depression levels in relatively normal people but also relieve depression in individual with major depression. They can even help in cases where drugs fail to relieve the depression. In addition, mindfulness practices can reduce the likelihood of a relapse after successful treatment for depression. In other words, mindfulness is an effective treatment either alone or in combination with drugs for depression.
In the last few decades it has become increasingly clear that the brain is very plastic and can be reshaped by what we do and what we experience. This has been called neuroplasticity. Contemplative practices have been shown to produce neuroplastic change altering the brain. They tend to increase the size, activity, and connectivity of areas of the brain that are important for attention, and emotion regulation while reducing the size, activity, and connectivity of areas of the brain that are involved in mind wandering and self-centered thinking, daydreaming, and rumination.
Mindfulness practices appear to take advantage of neuroplasticity to act upon the chemistry of the brain and brain electrical activity to help relieve depression. Hence, it makes sense that there should be further research on the effects of mindfulness on the brain and depression to better understand the mechanisms of action of mindfulness and potentially optimize treatment. In today’s Research News article “State and Training Effects of Mindfulness Meditation on Brain Networks Reflect Neuronal Mechanisms of Its Antidepressant Effect”
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4779536/
Yang and colleagues trained meditation naive college students for 8-weeks with a mindfulness program based upon a combination of Mindfulness Based Stress Reduction (MBSR) and Acceptance and Commitment Therapy (ACT). Functional Magnetic Resonance Imaging (f-MRI) brain scans were performed before training and 40 days later both at rest and during meditation. The students emotional state and depression levels were also measured before and after training.
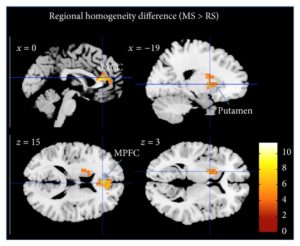
After mindfulness training there was a 45% reduction in depression, a 21% reduction in trait anxiety, and a small reduction in tension. The brain was also found to be changed at rest after training. The changes were many and diverse. But arguably the most interesting change was a reduction in the functional connectivity between the pregenual anterior cingulate and dorsal medical prefrontal cortex. The anterior cingulate cortex is part of what is called the default mode network that is activated during mind wandering and emotionality. It is involved in major depression and the loss of emotionality, so called flat affect, that characterizes depression. On the other hand, the dorsal medical prefrontal cortex is involved in focused attention, cognitive control, and emotion regulation. These results are very complex and must be interpreted cautiously. But, it appears that meditation training reduces the ability of areas involved in depression from affecting areas involved in thought and emotion. This is a potential route for mindfulness affects in relieving depression.
Regardless, it’s clear that mindfulness can change the depressed brain.
“We can intentionally shape the direction of plasticity changes in our brain. By focusing on wholesome thoughts, for example, and directing our intentions in those ways, we can potentially influence the plasticity of our brains and shape them in ways that can be beneficial.” – Richie Davidson
CMCS – Center for Mindfulness and Contemplative Studies
Study Summary
Yang, C.-C., Barrós-Loscertales, A., Pinazo, D., Ventura-Campos, N., Borchardt, V., Bustamante, J.-C., … Walter, M. (2016). State and Training Effects of Mindfulness Meditation on Brain Networks Reflect Neuronal Mechanisms of Its Antidepressant Effect. Neural Plasticity, 2016, 9504642. http://doi.org/10.1155/2016/9504642
Abstract
The topic of investigating how mindfulness meditation training can have antidepressant effects via plastic changes in both resting state and meditation state brain activity is important in the rapidly emerging field of neuroplasticity. In the present study, we used a longitudinal design investigating resting state fMRI both before and after 40 days of meditation training in 13 novices. After training, we compared differences in network connectivity between rest and meditation using common resting state functional connectivity methods. Interregional methods were paired with local measures such as Regional Homogeneity. As expected, significant differences in functional connectivity both between states (rest versus meditation) and between time points (before versus after training) were observed. During meditation, the internal consistency in the precuneus and the temporoparietal junction increased, while the internal consistency of frontal brain regions decreased. A follow-up analysis of regional connectivity of the dorsal anterior cingulate cortex further revealed reduced connectivity with anterior insula during meditation. After meditation training, reduced resting state functional connectivity between the pregenual anterior cingulate and dorsal medical prefrontal cortex was observed. Most importantly, significantly reduced depression/anxiety scores were observed after training. Hence, these findings suggest that mindfulness meditation might be of therapeutic use by inducing plasticity related network changes altering the neuronal basis of affective disorders such as depression.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4779536/