Prevent Depression and Dementia-Related Behavioral Symptoms in Alzheimer’s Disease with Mindfulness
By John M. de Castro, Ph.D.
“Alzheimer’s is not about the past—the successes, the accolades, the accomplishments… Alzheimer’s is about the present and the struggle, the scrappy brawl, the fight to live with a disease. It’s being in the present, the relationships, the experiences, which is the core of life, the courage to live in the soul”. – Greg O’Brien
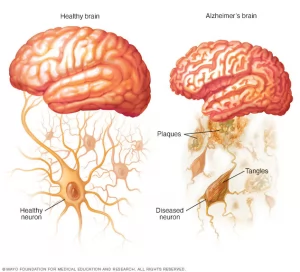
The normal aging process involves a systematic progressive decline in every system in the body, the brain included. The elderly frequently have problems with attention, thinking, and memory, known as mild cognitive impairment. But sometimes the decline is rapid and results in dementia; a progressive loss of mental function produced by degenerative diseases of the brain. It is quite common with about 3% of adults ages 70 to 74, 22% of adults ages 85 to 89 and 33% of adults ages 90 and older. Between 60% to 80% of dementia cases are classified as Alzheimer’s Disease. Depression is a common symptom.
An encouraging new development is that mindfulness practices such as meditation training and mindful movement practices can significantly reduce these declines in cognitive ability. In addition, it has been found that mindfulness practices reduce the deterioration of the brain that occurs with aging restraining the loss of neural tissue. This suggests that mindfulness may also help to relieve some of the psychological symptoms of the disease; particularly mindfulness practices ability to prevent the development of depression in patients with mild to moderate Alzheimer’s Disease.
In today’s Research News article “Mindfulness Prevents Depression and Psychopathology in Elderly People with Mild to Moderate Alzheimer’s Disease: A Randomized Clinical Trial” (See summary below or view the full text of the study at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9881020/ ) Quintana-Hernández and colleagues recruited patients with mild to moderate Alzheimer’s Disease who were not showing depressive symptoms and randomly assigned them to receive either no treatment, mindfulness practice (Mindfulness-based Alzheimer’s Stimulation), cognitive stimulation, or progressive muscle relaxation. They were provided with three weekly sessions over 2 years. Mindfulness-based Alzheimer’s Stimulation involves caregiver and patient joint activities emphasizing present moment awareness.
The participants were measured at baseline and every 6 months thereafter for depression, and caregiver rated dementia-related behavioral symptoms, including delusions, hallucinations, agitation/aggression, dysphoria, anxiety, euphoria, apathy, disinhibition, irritability/lability, aberrant motor activity, night-time behavioral disturbances and appetite and eating abnormalities.
They found that, over the 2-year study period, mindfulness training and practice prevented the onset of depression and dementia-related behavioral symptoms in these patients while these symptoms increased progressively and significantly in all other groups.
These findings are remarkable and demonstrate that mindfulness training can prevent the development of depression and neuropsychiatric symptoms in early-stage Alzheimer’s Disease patients over a substantial period of time. This suggests that mindfulness training should be incorporated into the routine treatment of patients with mild to moderate Alzheimer’s Disease.
“You have to be patient with Alzheimer’s. Once you understand that it’s a medical condition, you become a little more compassionate. You get less frustrated.” – Kim Campbell
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on the Contemplative Studies Blog http://contemplative-studies.org
Study Summary
Quintana-Hernández DJ, Rojas-Hernández J, Santana-Del Pino A, Céspedes Suárez C, Pellejero Silva M, Miró-Barrachina MT, Ibáñez Fernández I, Estupiñán López JA, Borkel LF. Mindfulness Prevents Depression and Psychopathology in Elderly People with Mild to Moderate Alzheimer’s Disease: A Randomized Clinical Trial. J Alzheimers Dis. 2023;91(1):471-481. doi: 10.3233/JAD-220889. PMID: 36442199; PMCID: PMC9881020.
Background:
This longitudinal study addressed whether mindfulness practice prevents psychological and behavioral symptoms, especially mood disorders, in Alzheimer’s disease (AD).
Objective:
To assess the incidence of depression in the course of AD and to determine which non-pharmacological treatment (NPT) is most effective in preventing psychopathological symptoms.
Methods:
We conducted a longitudinal, non-inferiority and equivalence randomized clinical trial, repeated-measures design, with a control group and three experimental treatments: mindfulness, cognitive stimulation, and relaxation. Each experimental group performed three weekly sessions for two years. The pharmacological treatment of all participants was donepezil (10 mg). Participants were patients with probable AD without diagnosed depression from the public neurology services of the Canary Health Service, Spain. Psychological evaluation was performed using the Geriatric Depression Scale (GDS), Hamilton Depression Rating Scale (HDRS), and Neuropsychiatric Inventory (NPI-Q). The statistical analysis included only patients who attended at least 75% of the sessions. A nonparametric, repeated-measures analysis was performed with Kruskal-Wallis H test and between-group differences with Mann-Whitney U test with Bonferroni correction (p < 0.008). Effect size was calculated with partial eta-squared.
Results:
The results showed significant differences with large effect sizes (η2p>0.14) between mindfulness and the rest of the experimental groups as well as the control in the GDS, HDRS, and NPI-Q scales.
Conclusion:
Compared to the other experimental groups, only mindfulness prevented the onset of depression and other psychopathologies in early-stage AD. Based on its effectiveness in maintaining cognitive functions and preventing psychopathology, we recommend mindfulness as the first-choice NPT for mild to moderate AD.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9881020/