Reduce Blood Pressure in Patients with Noncommunicable Diseases with Mindfulness
By John M. de Castro, Ph.D.
“mindfulness practice can be an effective way to reduce blood pressure (and along with it, the risk of stroke or heart attack).” – NICABM
High Blood Pressure (Hypertension) is an insidious disease because there are no overt symptoms. The individual feels fine. But it can be deadly as more than 360,000 American deaths, roughly 1,000 deaths each day, had high blood pressure as a primary or contributing cause. In addition, hypertension markedly increases the risk heart attack, stroke, heart failure, and kidney disease. It is also a very common disorder with about 70 million American adults (29%) having high blood pressure and only about half (52%) of people with high blood pressure have their condition under control. Treatment frequently includes antihypertensive drugs. But these medications often have adverse side effects. So, patients feel lousy when taking the drugs, but fine when they’re not. So, compliance is a major issue with many patients not taking the drugs regularly or stopping entirely.
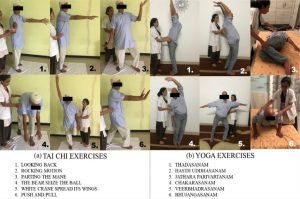
Obviously, there is a need for alternative to drug treatments for hypertension. Mindfulness practices have been shown to aid in controlling hypertension. Indeed, meditation, tai chi, and yoga, have also been shown to be helpful for heart health. Hypertension is frequently cooccurring with in patients with non-communicable diseases. In today’s Research News article “Mindfulness interventions reduce blood pressure in patients with non-communicable diseases: A systematic review and meta-analysis.” (See summary below or view the full text of the study at: https://www.ncbi.nlm.nih.gov/pmc), Intarakamhang and colleagues review, summarize and perform a meta-analysis of the effectiveness of mindfulness training in reducing blood pressure in patients with non-communicable diseases.
They defined non-communicable diseases (NCDs) to include cancers, cardiovascular diseases, respiratory diseases and diabetes and identified 14 published controlled studies including a total of 1117 patients. They report that the studies found that mindfulness training significantly reduced both systolic and diastolic blood pressure in the patients with NCDs.
The results are compatible with previous findings that mindfulness training reduces blood pressure in a wide variety of healthy and ill individuals. The present study demonstrates that mindfulness training is effective in reducing blood pressure in patients with non-communicable diseases (NCDs). This is reasonable given that mindfulness training has been shown to improve the symptoms of patients with the included NCDs, cancers, cardiovascular diseases, respiratory diseases and diabetes.
There are a number of possible mechanisms for this blood pressure reduction. Mindfulness training is known to reduce the physiological and psychological responses to stress and this may in turn lower blood pressure. Also mindfulness training has been shown to affect the autonomic nervous system increasing parasympathetic activity that tends to reduce blood pressure.
So, reduce blood pressure in patients with noncommunicable diseases with mindfulness.
“The hope is that if we can start mindfulness training early in life, we can promote a trajectory of healthy aging across the rest of people’s lives. That will reduce their chances of getting high blood pressure in the first place.” – Eric Loucks
CMCS – Center for Mindfulness and Contemplative Studies
This and other Contemplative Studies posts are also available on Google+ https://plus.google.com/106784388191201299496/posts and on Twitter @MindfulResearch
Study Summary
Intarakamhang, U., Macaskill, A., & Prasittichok, P. (2020). Mindfulness interventions reduce blood pressure in patients with non-communicable diseases: A systematic review and meta-analysis. Heliyon, 6(4), e03834. https://doi.org/10.1016/j.heliyon.2020.e03834
Abstract
Purpose
Mindfulness based interventions (MBIs) are an emerging area of empirical study, not only in positive psychology, but also in clinical health care. This research aims to synthesize the evidence about whether MBIs reduce blood pressure (BP) in patients with non-communicable diseases (NCDs).
Methods
Relevant studies were identified via PubMed, the Cochrane Library, Embase and the CINAHL database between 2009 and 2019. The papers selected focused on mindfulness and the effect of these on the BP of patients with NCDs. The change in SBP and DBP were meta-analyzed, stratified by type of intervention (Breathing awareness meditation (BAM), Mindfulness Meditation (MM), and Mindfulness-based Stress Reduction (MBSR).
Results
Fourteen articles met eligibility criteria and were included in the final review. Among the studies using the type and duration of intervention, systolic BP was reduced after the mindfulness-based stress reduction for 8 weeks (-6.90 mmHg [95% CI: -10.82, -2.97], p < .050), followed by the breathing awareness meditation for 12 weeks (-4.10 mmHg [95% CI: -7.54, -0.66], p < .050) and the mindfulness-based intervention for 8 weeks (-2.69 mmHg [95% CI: -3.90, -1.49], p < .050) whereas diastolic BP was reduced after the mindfulness-based stress reduction for 8 weeks (-2.45 mmHg [95% CI: -3.74, -1.17], p < .050) and the mindfulness-based intervention for 8 weeks (-2.24 mmHg [95% CI: -3.22, -1.26], p < .050).
Conclusion
MBIs can provide effective alternative therapies to assist in blood pressure reduction for patients with NCDs.
https://www.ncbi.nlm.nih.gov/pmc